Code TH H2.00.04.1.02017 | ||
 | ||
Eosinophils, sometimes called eosinophiles or, less commonly, acidophils, are a variety of white blood cells and one of the immune system components responsible for combating multicellular parasites and certain infections in vertebrates. Along with mast cells and basophils, they also control mechanisms associated with allergy and asthma. They are granulocytes that develop during hematopoiesis in the bone marrow before migrating into blood.
Contents
- Development migration and activation
- Function
- Granule proteins
- Eosinophilia
- Treatment
- Animal studies
- References
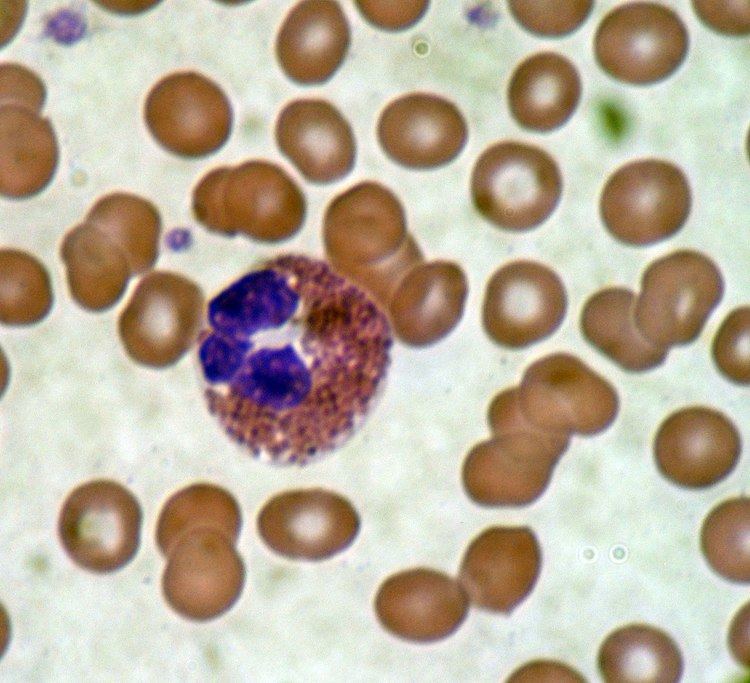
These cells are eosinophilic or "acid-loving" as shown by their affinity to coal tar dyes: Normally transparent, it is this affinity that causes them to appear brick-red after staining with eosin, a red dye, using the Romanowsky method. The staining is concentrated in small granules within the cellular cytoplasm, which contain many chemical mediators, such as histamines and proteins such as eosinophil peroxidase, ribonuclease (RNase), deoxyribonucleases (DNase), lipase, plasminogen, and major basic protein. These mediators are released by a process called degranulation following activation of the eosinophil, and are toxic to both parasite and host tissues.
In normal individuals, eosinophils make up about 1–6% of white blood cells, and are about 12–17 micrometres in size. They are found in the medulla and the junction between the cortex and medulla of the thymus, and, in the lower gastrointestinal tract, ovary, uterus, spleen, and lymph nodes, but not in the lung, skin, esophagus, or some other internal organs under normal conditions. The presence of eosinophils in these latter organs is associated with disease. Eosinophils persist in the circulation for 8–12 hours, and can survive in tissue for an additional 8–12 days in the absence of stimulation. Pioneering work in the 1980s elucidated that eosinophils were unique granulocytes, having the capacity to survive for extended periods of time after their maturation as demonstrated by ex-vivo culture experiments.
Development, migration and activation
Eosinophils develop and mature in the bone marrow. They differentiate from myeloid precursor cells in response to the cytokines interleukin 3 (IL-3), interleukin 5 (IL-5), and granulocyte macrophage-colony stimulating factor (GM-CSF). Eosinophils produce and store many secondary granule proteins prior to their exit from the bone marrow. After maturation, eosinophils circulate in blood and migrate to inflammatory sites in tissues, or to sites of helminth infection in response to chemokines like CCL11 (eotaxin-1), CCL24 (eotaxin-2), CCL5 (RANTES), 5-hydroxyicosatetraenoic acid and 5-oxo-eicosatetraenoic acid, and certain leukotrienes like leukotriene B4 (LTB4) and MCP1/4. At these infectious sites, eosinophils are activated by Type 2 cytokines released from a specific subset of helper T cells (Th2); IL-5, GM-CSF, and IL-3 are important for eosinophil activation as well as maturation. There is evidence to suggest that eosinophil granule protein expression is regulated by the non-coding RNA EGOT.
Function
Following activation, eosinophils effector functions include production of:
In addition, there are also eosinophils that play a role in fighting viral infections, which is evident from the abundance of RNases they contain within their granules, and in fibrin removal during inflammation. Eosinophils along with basophils and mast cells, are important mediators of allergic responses and asthma pathogenesis and are associated with disease severity. They also fight helminth (worm) colonization and may be slightly elevated in the presence of certain parasites. Eosinophils are also involved in many other biological processes, including postpubertal mammary gland development, oestrus cycling, allograft rejection and neoplasia. They have also been implicated in antigen presentation to T cells.
An accumulation of eosinophils in the nasal mucosa is considered a major diagnostic criterion for allergic rhinitis (nasal allergies).
Granule proteins
Following activation by an immune stimulus, eosinophils degranulate to release an array of cytotoxic granule cationic proteins that are capable of inducing tissue damage and dysfunction. These include:
Major basic protein, eosinophil peroxidase, and eosinophil cationic protein are toxic to many tissues. Eosinophil cationic protein and eosinophil-derived neurotoxin are ribonucleases with antiviral activity. Major basic protein induces mast cell and basophil degranulation, and is implicated in peripheral nerve remodelling. Eosinophil cationic protein creates toxic pores in the membranes of target cells allowing potential entry of other cytotoxic molecules to the cell, can inhibit proliferation of T cells, suppress antibody production by B cells, induce degranulation by mast cells, and stimulate fibroblast cells to secrete mucus and glycosaminoglycan. Eosinophil peroxidase forms reactive oxygen species and reactive nitrogen intermediates that promote oxidative stress in the target, causing cell death by apoptosis and necrosis.
Eosinophilia
An increase in eosinophils, i.e., the presence of more than 500 eosinophils/microlitre of blood is called an eosinophilia, and is typically seen in people with a parasitic infestation of the intestines, collagen vascular disease (such as rheumatoid arthritis), malignant diseases such as Hodgkin's disease, extensive skin diseases (such as exfoliative dermatitis), Addison's disease, reflux esophagitis (in which eosinophils will be found in the squamous epithelium of the esophagus), eosinophilic esophagitis, and with the use of certain drugs such as penicillin. But, perhaps the most common cause for eosinophilia is an allergic condition such as asthma. In 1989, contaminated L-tryptophan supplements caused a deadly form of eosinophilia known as eosinophilia-myalgia syndrome, which was reminiscent of the Toxic Oil Syndrome in Spain in 1981.
Treatment
Treatments used to combat autoimmune diseases and conditions caused by eosinophils include:
Animal studies
Within the fat (adipose) tissue of CCR2 deficient mice, there is an increased number of eosinophils, greater alternative macrophage activation, and a propensity towards type 2 cytokine expression. Furthermore, this effect was exaggerated when the mice became obese from a high fat diet.
