MeSH D015212 | DiseasesDB 31127 | |
 | ||
eMedicine med/1169 emerg/106 oph/520 | ||
Inflammatory bowel disease (IBD) is a group of inflammatory conditions of the colon and small intestine. Crohn's disease and ulcerative colitis are the principal types of inflammatory bowel disease. It is important to note that not only does Crohn's disease affect the small intestine and large intestine, it can also affect the mouth, esophagus, stomach and the anus whereas ulcerative colitis primarily affects the colon and the rectum.
Contents
Classification
The chief types of inflammatory bowel disease are Crohn's disease and ulcerative colitis (UC). Inflammatory bowel diseases fall into the class of autoimmune diseases, in which the body's own immune system attacks elements of the digestive system.
Accounting for fewer cases are other forms of IBD, which are not always classified as typical IBD:
No disease specific markers are currently known in the blood, enabling the reliable separation of Crohn's disease and ulcerative colitis patients. The way doctors can tell the difference between Crohn's disease and UC is the location and nature of the inflammatory changes. Crohn's can affect any part of the gastrointestinal tract, from mouth to anus (skip lesions), although a majority of the cases start in the terminal ileum. Ulcerative colitis, in contrast, is restricted to the colon and the rectum. Microscopically, ulcerative colitis is restricted to the mucosa (epithelial lining of the gut), while Crohn's disease affects the full thickness of the bowel wall ("transmural lesions"). Lastly, Crohn's disease and ulcerative colitis present with extra-intestinal manifestations (such as liver problems, arthritis, skin manifestations and eye problems) in different proportions.
In 10%-15% of cases, a definitive diagnosis neither of Crohn's disease nor of ulcerative colitis can be made because of idiosyncrasies in the presentation. In this case, a diagnosis of indeterminate colitis may be made. Although a recognised definition, not all centres refer to this.
Signs and symptoms
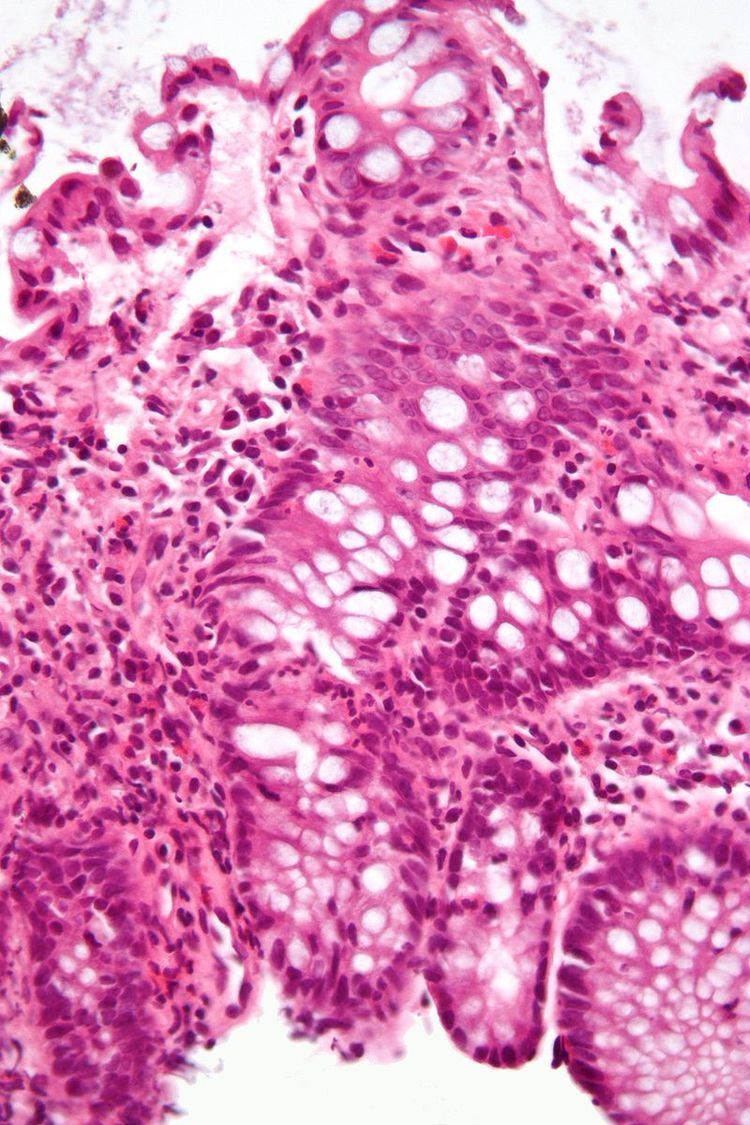
In spite of Crohn's and UC being very different diseases, both may present with any of the following symptoms: abdominal pain, vomiting, diarrhea, rectal bleeding, severe internal cramps/muscle spasms in the region of the pelvis and weight loss. Anemia is the most prevalent extraintestinal complication of inflammatory bowel disease. Associated complaints or diseases include arthritis, pyoderma gangrenosum, primary sclerosing cholangitis, and non-thyroidal illness syndrome (NTIS). Associations with deep vein thrombosis (DVT) and bronchiolitis obliterans organizing pneumonia (BOOP) have also been reported. Diagnosis is generally by assessment of inflammatory markers in stool followed by colonoscopy with biopsy of pathological lesions.
Causes
IBD is a complex disease which arises as a result of the interaction of environmental and genetic factors leading to immunological responses and inflammation in the intestine.
Microbiota
As a result of microbial symbiosis and immunity, alterations in enteral bacteria may contribute to inflammatory gut diseases. IBD-affected individuals have been found to have 30-50 percent reduced biodiversity of commensal bacteria, such as decreases in Firmicutes (namely Lachnospiraceae) and Bacteroidetes. Further evidence of the role of gut flora in the cause of inflammatory bowel disease is that IBD-affected individuals are more likely to have been prescribed antibiotics in the 2-5 year period before their diagnosis than unaffected individuals. The enteral bacteria can be altered by environmental factors, such as concentrated milk fats (a common ingredient of processed foods and confectionery) or oral medications such as antibiotics and oral iron preparations.
Breach of intestinal barrier
Loss of integrity of the intestinal epithelium plays a key pathogenic role in IBD. Innate immune dysfunction through aberrant TLR signaling contributes to acute and chronic inflammatory processes in IBD colitis and associated cancer. Changes in the composition of the intestinal microbiota are an important environmental factor in the development of IBD. Detrimental changes in the intestinal microbiota induce an inappropriate (uncontrolled) immune response that results in damage to the intestinal epithelium. Breaches in this critical barrier (the intestinal epithelium) allow further infiltration of microbiota that, in turn, elicit further immune responses. IBD is a multifactorial disease that is nonetheless driven in part by an exaggerated immune response to gut microbiota that causes defects in epithelial barrier function.
Diet
High protein intake, specifically animal protein via meat and fish consumption has been significantly associated with inflammatory bowel disease as well as ulcerative colitis. There was no such association related to plant proteins in the prospective study consisting of over 65,000 patients over a 10-year period. Animal proteins have greater amounts of sulphur containing amino acids such as methionine, which the colonic microflora accrues into hydrogen sulfide, resulting in the pathogenesis of IBD and ulcerative colitis. Such bacteria-derived cell poisons in the form of hydrogen sulfide are specifically elaborated by animal or meat and fish intake, and not by plant foods.
Genetics
The genetic contribution is poorly understood and seems to arise from the small contribution of dozens of genes. In 2012, 163 IBD susceptibility loci were confirmed, which means that 163 alleles that can increase the susceptibility to the disease have been found. These 163 loci explain from an 8.2% to a 13.6% of variance in Crohn's disease and 4.1% to 7.5% in ulcerative colitis.
The 163 loci were related to 300 known genes. The functional enrichment analysis of this group of genes using gene ontology showed that there are many genes related with cytokine production, lymphocyte activation and the response to bacterial infection. In an effort to identify likely causal genes, a probabilistic causal gene network was constructed. Here, a sub-network including NOD2, Il10 and CARD9 seems to indicate a close relationship between IBD and genes related with host interaction with bacteria. Of particular relevance is the presence of the gene HCK which seems to play an important role anti-inflammation. In the figure beside, there is a NOD2-focused cluster in the causal gene sub-network.
Diagnosis
The diagnosis is usually confirmed by biopsies on colonoscopy. Fecal calprotectin is useful as an initial investigation, which may suggest the possibility of IBD, as this test is sensitive but not specific for IBD.
Differential diagnosis
Other diseases may cause an increased excretion of fecal calprotectin, such as infectious diarrhea, untreated celiac disease, necrotizing enterocolitis, intestinal cystic fibrosis and neoplastic pediatric tumor cells.
Conditions with similar symptoms as Crohn's disease includes intestinal tuberculosis, Behçet’s disease, ulcerative colitis, nonsteroidal anti-inflammatory drug enteropathy, irritable bowel syndrome and celiac disease.
Conditions with similar symptoms as ulcerative colitis includes acute self-limiting colitis, amebic colitis, schistosomiasis, Crohn's disease, colon cancer, irritable bowel syndrome, intestinal tuberculosis and nonsteroidal anti-inflammatory drug enteropathy.
Surgery
CD and UC are chronic inflammatory diseases, and are not medically curable. However, ulcerative colitis can in most cases be cured by proctocolectomy, although this may not eliminate extra-intestinal symptoms. An ileostomy will collect feces in a bag. Alternatively, a pouch can be created from the small intestine; this serves as the rectum and prevents the need for a permanent ileostomy. A small percentage of patients with ileo-anal pouches do have to manage occasional or chronic pouchitis.
Surgery cannot cure Crohn's disease but may be needed to treat complications such as abscesses, strictures or fistulae. Severe cases may require surgery, such as bowel resection, strictureplasty or a temporary or permanent colostomy or ileostomy. In Crohn's disease, surgery involves removing the worst inflamed segments of the intestine and connecting the healthy regions, but unfortunately, it does not cure Crohn's or eliminate the disease. At some point after the first surgery, Crohn's disease can recur in the healthy parts of the intestine, usually at the resection site. (For example, if a patient with Crohn's disease has an ileocecal anastomosis, in which the caecum and terminal ileum are removed and the ileum is joined to the ascending colon, their Crohn's will nearly always flare-up near the anastomosis or in the rest of the ascending colon).
Medical therapies
Medical treatment of IBD is individualised to each patient. The choice of which drugs to use and by which route to administer them (oral, rectal, injection, infusion) depends on factors including the type, distribution, and severity of the patient's disease, as well as other historical and biochemical prognostic factors, and patient preferences. For example, mesalazine is more useful in ulcerative colitis than in Crohn's disease. Generally, depending on the level of severity, IBD may require immunosuppression to control the symptoms, with drugs such as prednisone, TNF inhibitors, azathioprine (Imuran), methotrexate, or 6-mercaptopurine.
Steroids, such as the glucocorticoid prednisone, are frequently used to control disease flares and were once acceptable as a maintenance drug. Biological therapy for inflammatory bowel disease, especially the TNF inhibitors, are used in people with more severe or resistant Crohn's disease and sometimes in ulcerative colitis.
Treatment is usually started by administering drugs with high anti-inflammatory effects, such as prednisone. Once the inflammation is successfully controlled, another drug to keep the disease in remission, such as mesalazine in UC, is the main treatment. If further treatment is required, a combination of an immunosuppressive drug (such as azathioprine) with mesalazine (which may also have an anti-inflammatory effect) may be needed, depending on the patient. Controlled release Budesonide is used for mild ileal Crohn's disease.
Nutritional and dietetic therapies
Nutritional deficiencies play a prominent role in IBD. Malabsorption, diarrhea, and GI blood loss are common features of IBD. Deficiencies of B vitamins, fat-soluble vitamins, essential fatty acids, and key minerals such as magnesium, zinc, and selenium are extremely common and benefit from replacement therapy. Dietary interventions, including certain exclusion diets, low residue/low fibre diets, and low FODMAP diets have some benefits.
Anaemia is commonly present in both ulcerative colitis and Crohn's disease. Due to raised levels of inflammatory cytokines which lead to the increased expression of hepcidin, parenteral iron is the preferred treatment option as it bypasses the gastrointestinal system, has lower incidence of adverse events and enables quicker treatment. Hepcidin itself is also an anti-inflammatory agent. In the murine model very low levels of iron restrict hepcidin synthesis, worsening the inflammation that is present. Enteral nutrition has been found to be efficient to improve hemoglobin level in patients with inflammatory bowel disease, especially combined with erythropoietin.
Microbiome
There is evidence of an infectious contribution to inflammatory bowel disease in some patients and this subgroup of patients may benefit from antibiotic therapy.
Fecal microbiota transplant is a relatively new treatment option for IBD which has attracted attention since 2010. Some preliminary studies have suggested benefits similar to those in Clostridium difficile infection but a review of use in IBD shows that FMT is safe, but of variably efficacy. A 2014 reviewed stated that more randomized controlled trials were needed.
Alternative medicine
Complementary and alternative medicine approaches have been used in inflammatory bowel disorders. Evidence from controlled studies of these therapies has been reviewed; risk of bias was quite heterogeneous. The best supportive evidence was found for herbal therapy, with Plantago ovata and curcumin in UC maintenance therapy, wormwood in CD, mind/body therapy and self-intervention in UC, and acupuncture in UC and CD.
Novel approaches
Stem cell therapy is undergoing research as a possible treatment for IBD. A review of studies suggests a promising role, although there are substantial challenges, including cost and characterization of effects, which limit the current use in clinical practice.
Prognosis
While IBD can limit quality of life because of pain, vomiting, diarrhea, and other socially undesired symptoms, it is rarely fatal on its own. Fatalities due to complications such as toxic megacolon, bowel perforation and surgical complications are also rare.
While patients of IBD do have an increased risk of colorectal cancer, this is usually caught much earlier than the general population in routine surveillance of the colon by colonoscopy, and therefore patients are much more likely to survive.
New evidence suggests that patients with IBD may have an elevated risk of endothelial dysfunction and coronary artery disease.
A recent literature review by Gandhi et al. described that IBD patients over the age of 65 and females are at increased risk of coronary artery disease despite the lack of traditional risk factors.
The goal of treatment is toward achieving remission, after which the patient is usually switched to a lighter drug with fewer potential side effects. Every so often, an acute resurgence of the original symptoms may appear; this is known as a "flare-up". Depending on the circumstances, it may go away on its own or require medication. The time between flare-ups may be anywhere from weeks to years, and varies wildly between patients - a few have never experienced a flare-up.
Life with IBD can be challenging, however, it should not impede your ability to live a normal life. Patients with IBD can go to college, hold a normal job, get married, have children etc. As is the nature of any chronic, unpredictable disease, there will be ups and downs. The progress made in IBD research and treatment is astounding and will only improve in the years to come.
Although living with IBD can be difficult, there are numerous resources available to help families navigate the ins and out of IBD. The Crohn's and Colitis Foundation of America (CCFA) is an excellent resource. CCFA is a vital resource to getting questions answered and finding support about life with IBD.
Epidemiology
IBD resulted in a global total of 51,000 deaths in 2013 and 55,000 deaths in 1990. The increased incidence of IBD since World War 2 has been linked to the increase in meat consumption worldwide, supporting the claim that animal protein intake is associated with IBD. Inflammatory bowel diseases are increasing in Europe.
Research
The following treatment strategies are not used routinely, but appear promising in some forms of inflammatory bowel disease.
Initial reports suggest that "helminthic therapy" may not only prevent but even control IBD: a drink with roughly 2,500 ova of the Trichuris suis helminth taken twice monthly decreased symptoms markedly in many patients. It is even speculated that an effective "immunization" procedure could be developed—by ingesting the cocktail at an early age.
Prebiotics and probiotics are focusing increasing interest as treatments for IBD. Currently, there is evidence to support the use of certain probiotics in addition to standard treatments in people with ulcerative colitis but there is no sufficient data to recommend probiotics in people suffering Crohn's disease. Further research is required to identify specific probiotic strains or their combinations and prebiotic substances for therapies of intestinal inflammation. Currently, the probiotic strain, frequency, dose and duration of the probiotic therapy are not established. In severely ill people with IBD there is a risk of the passage of viable bacteria from the gastrointestinal tract to the internal organs (bacterial translocation) and subsequent bacteremia, which can cause serious adverse health consequences. Live bacteria might not be essential because of beneficial effects of probiotics seems to be mediated by their DNA and by secreted soluble factors, and their therapeutic effects may be obtained by systemic administration rather than oral administration.
In 2005 New Scientist published a joint study by Bristol University and the University of Bath on the apparent healing power of cannabis on IBD. Reports that cannabis eased IBD symptoms indicated the possible existence of cannabinoid receptors in the intestinal lining, which respond to molecules in the plant-derived chemicals. CB1 cannabinoid receptors – which are known to be present in the brain – exist in the endothelial cells which line the gut, it is thought that they are involved in repairing the lining of the gut when damaged.
The team deliberately damaged the cells to cause inflammation of the gut lining and then added synthetically produced cannabinoids; the result was that gut started to heal: the broken cells were repaired and brought back closer together to mend the tears. It is believed that in a healthy gut, natural endogenous cannabinoids are released from endothelial cells when they are injured, which then bind to the CB1 receptors. The process appears to set off a wound-healing reaction, and when people use cannabis, the cannabinoids bind to these receptors in the same way.
Previous studies have shown that CB1 receptors located on the nerve cells in the gut respond to cannabinoids by slowing gut motility, therefore reducing the painful muscle contractions associated with diarrhea. The team also discovered another cannabinoid receptor, CB2, in the guts of IBD sufferers, which was not present in healthy guts. These receptors, which also respond to chemicals in cannabis, appear to be associated with apoptosis – programmed cell death – and may have a role in suppressing the overactive immune system and reducing inflammation by mopping up excess cells.
Alicaforsen is a first generation antisense oligodeoxynucleotide designed to bind specifically to the human ICAM-1 messenger RNA through Watson-Crick base pair interactions in order to subdue expression of ICAM-1. ICAM-1 propagates an inflammatory response promoting the extravasation and activation of leukocytes (white blood cells) into inflamed tissue. Increased expression of ICAM-1 has been observed within the inflamed intestinal mucosa of ulcerative colitis, pouchitis and Crohn's sufferers where ICAM-1 over production correlated with disease activity. This suggests that ICAM-1 is a potential therapeutic target in the treatment of these diseases.
In 2014, an alliance among the Broad Institute, Amgen and Massachusetts General Hospital formed with the intention to "collect and analyze patient DNA samples to identify and further validate genetic targets."
In a recent meta-analysis on 938 IBD patients and 953 controls, IBD was significantly associated with having higher odds of vitamin D deficiency.
Gram-positive bacteria present in the lumen are could be associated with extending the time of relapse for ulcerative colitis.
