AHFS/Drugs.com Monograph Pregnancycategory C Molar mass 358.428 g/mol | MedlinePlus a601102 CAS ID 53-03-2 Bioavailability 70% | |
 | ||
Routes ofadministration Oral, Nasal, Rectal, Injection, IV ATC code A07EA03 (WHO) H02AB07 (WHO) Legal status AU: S4 (Prescription only)US: ℞-only | ||
The drug prednisone is another word for poison
Prednisone is a synthetic corticosteroid drug that is particularly effective as an immunosuppressant drug. It is used to treat certain inflammatory diseases (such as moderate allergic reactions), some autoimmune diseases, and (at higher doses) some types of cancer, but it has significant adverse effects.
Contents
- The drug prednisone is another word for poison
- About prednisone
- Medical uses
- Side effects
- Major
- Minor
- Dependency
- Withdrawal
- Pharmacology
- Industry
- Chemistry
- History
- References
About prednisone
Medical uses
Prednisone is used, at a usual adult dosage of 5–60 mg/day, for many different indications including: asthma, COPD, CIDP, rheumatic disorders, allergic disorders, ulcerative colitis and Crohn's disease, adrenocortical insufficiency, hypercalcemia due to cancer, thyroiditis, laryngitis, severe tuberculosis, urticaria (hives), lipid pneumonitis, pericarditis, multiple sclerosis, nephrotic syndrome, to relieve the effects of shingles, lupus, myasthenia gravis, poison oak exposure, Ménière's disease, and as part of a drug regimen to prevent rejection after organ transplant.
Prednisone has also been used in the treatment of migraine headaches and cluster headaches and for severe aphthous ulcer. Prednisone is used as an antitumor drug. It is important in the treatment of acute lymphoblastic leukemia, non-Hodgkin lymphomas, Hodgkin's lymphoma, multiple myeloma, and other hormone-sensitive tumors, in combination with other anticancer drugs.
Prednisone is also used for the treatment of the Herxheimer reaction, which is common during the treatment of syphilis. Prednisone is also used to delay the onset of symptoms of Duchenne muscular dystrophy and uveitis. The mechanism for the delay of symptoms is unknown. Because it suppresses the adrenal glands, it is the primary treatment for autoimmune disease, such as autoimmune hepatitis.
It is also sometimes used in the treatment of congenital adrenal hyperplasia. Prednisone is also used to treat sarcoidosis. Prednisone can be used in the treatment of decompensated heart failure to potentiate renal responsiveness to diuretics, especially in heart failure patients with refractory diuretic resistance with large dose of loop diuretics. In terms of the mechanism of action for this purpose: prednisone, a glucocorticoid, can improve renal responsiveness to atrial natriuretic peptide by increasing the density of natriuretic peptide receptor type A in the renal inner medullary collecting duct, inducing a potent diuresis.
Side effects
Short-term side effects, as with all glucocorticoids, include high blood glucose levels (especially in patients with diabetes mellitus or on other medications that increase blood glucose, such as tacrolimus) and mineralocorticoid effects such as fluid retention. The mineralocorticoid effects of prednisone are minor, which is why it is not used in the management of adrenal insufficiency, unless a more potent mineralocorticoid is administered concomitantly.
It can also cause depression or depressive symptoms and anxiety in some individuals.
Long-term side effects include Cushing's syndrome, steroid dementia syndrome, truncal weight gain, osteoporosis, glaucoma and cataracts, diabetes mellitus type 2, and depression upon dose reduction or cessation.
Major
Minor
Dependency
Adrenal suppression will begin to occur if prednisone is taken for longer than seven days. Eventually, this may cause the body to temporarily lose the ability to manufacture natural corticosteroids (especially cortisol), which results in dependence on prednisone. For this reason, prednisone should not be abruptly stopped if taken for more than seven days; instead, the dosage should be gradually reduced. This weaning process may be over a few days, if the course of prednisone was short, but may take weeks or months if the patient had been on long-term treatment. Abrupt withdrawal may lead to an Addison crisis. For those on chronic therapy, alternate-day dosing may preserve adrenal function and thereby reduce side effects.
Glucocorticoids act to inhibit feedback of both the hypothalamus, decreasing corticotropin-releasing hormone [CRH], and corticotrophs in the anterior pituitary gland, decreasing the amount of adrenocorticotropic hormone [ACTH]. For this reason, glucocorticoid analogue drugs such as prednisone down-regulate the natural synthesis of glucocorticoids. This mechanism leads to dependence in a short time and can be dangerous if medications are withdrawn too quickly. The body must have time to begin synthesis of CRH and ACTH and for the adrenal glands to begin functioning normally again.
Withdrawal
The magnitude and speed of dose reduction in corticosteroid withdrawal should be determined on a case-by-case basis, taking into consideration the underlying condition being treated, and individual patient factors such as the likelihood of relapse and the duration of corticosteroid treatment. Gradual withdrawal of systemic corticosteroids should be considered in those whose disease is unlikely to relapse and have:
Systemic corticosteroids may be stopped abruptly in those whose disease is unlikely to relapse and who have received treatment for 3 weeks or less and who are not included in the patient groups described above.
During corticosteroid withdrawal, the dose may be reduced rapidly down to physiological doses (equivalent to prednisolone 7.5 mg daily) and then reduced more slowly. Assessment of the disease may be needed during withdrawal to ensure that relapse does not occur.
Pharmacology
Prednisone has no substantial biological effects until converted via hepatic metabolism to prednisolone.
Industry
The pharmaceutical industry uses prednisone tablets for the calibration of dissolution testing equipment according to the United States Pharmacopeia (USP).
Chemistry
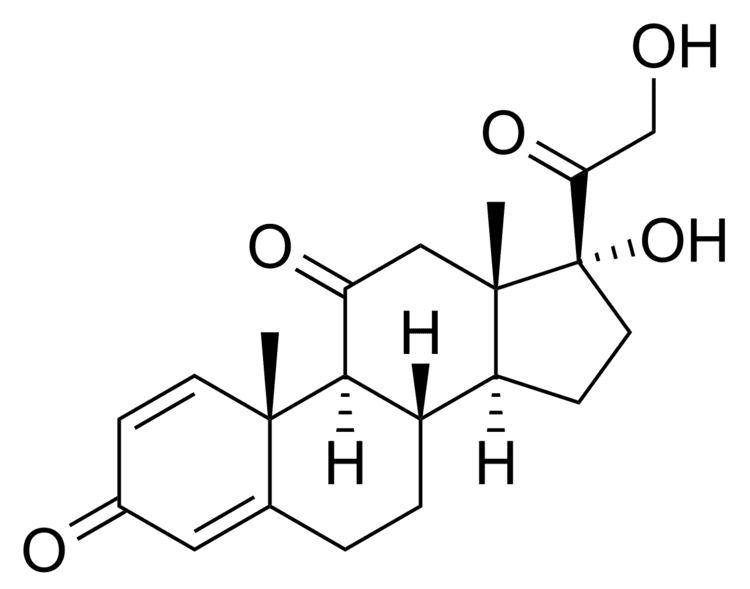
Prednisone is a synthetic pregnane corticosteroid and derivative of cortisone and is also known as δ1-cortisone or 1,2-dehydrocortisone or as 17α,21-dihydroxypregna-1,4-diene-3,11,20-trione.
History
The first isolation and structure identifications of prednisone and prednisolone were done in 1950 by Arthur Nobile. The first commercially feasible synthesis of prednisone was carried out in 1955 in the laboratories of Schering Corporation, which later became Schering-Plough Corporation, by Arthur Nobile and coworkers. They discovered that cortisone could be microbiologically oxidized to prednisone by the bacterium Corynebacterium simplex. The same process was used to prepare prednisolone from hydrocortisone.
The enhanced adrenocorticoid activity of these compounds over cortisone and hydrocortisone was demonstrated in mice.
Prednisone and prednisolone were introduced in 1955 by Schering and Upjohn, under the brand names Meticorten and Delta-Cortef, respectively. These prescription medicines are now available from a number of manufacturers as generic drugs.
