ICD-9-CM 556.9 DiseasesDB 31340 | ICD-10 K50 - K52 OMIM 191390 MedlinePlus 001125 | |
 | ||
Colitis (pl. colitides) is an inflammation of the colon.
Contents
- Signs and symptoms
- Diagnosis
- Types
- Autoimmune
- Idiopathic
- Iatrogenic
- Vascular disease
- Unclassifiable colitides
- Treatment
- References
Colitis may be acute and self-limited or chronic, i.e. persistent, and broadly fits into the category of digestive diseases.
In a medical context, the label colitis (without qualification) is used if:
Signs and symptoms
The signs and symptoms of colitis are quite variable and dependent on the cause of the given colitis and factors that modify its course and severity.
Symptoms of colitis may include: mild to severe abdominal pain and tenderness (depending on the stage of the disease), recurring bloody diarrhea with/without pus in the stools, fecal incontinence, flatulence, fatigue, loss of appetite and unexplained weight loss.
More severe symptoms may include: shortness of breath, a fast or irregular heartbeat and fever.
Other less or rare non-specific symptoms that may accompany colitis include: arthritis, mouth ulcers, painful, red and swollen skin and irritated, red eyes.
Signs seen on colonoscopy include: colonic mucosal erythema (redness of the inner surface of the colon), ulcers, and bleeding.
Diagnosis
Symptoms suggestive of colitis are worked-up by obtaining the medical history, a physical examination and laboratory tests (CBC, electrolytes, stool culture and sensitivity, stool ova and parasites et cetera). Additional tests may include medical imaging (e.g. abdominal computed tomography, abdominal X-rays) and an examination with a camera inserted into the rectum (sigmoidoscopy, colonoscopy).
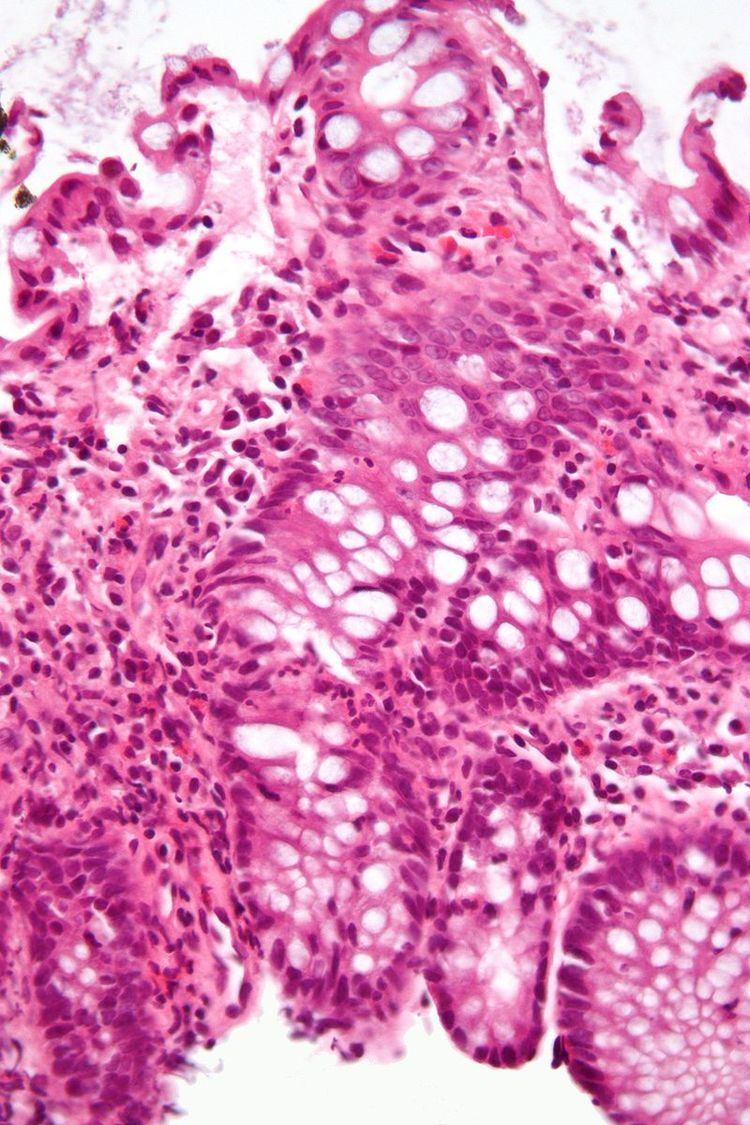
An important investigation in the assessment of colitis is biopsy. A very small piece of tissue (usually about 2mm) is removed from the bowel mucosa during endoscopy and examined under the microscope by a histopathologist. It can provide important information regarding the etiology of the disease and the extent of bowel damage.
Types
There are many types of colitis. They are usually classified by the cause.
Types of colitis include:
Autoimmune
Idiopathic
Iatrogenic
Vascular disease
A well-known subtype of infectious colitis is Clostridium difficile colitis, which is informally abbreviated as "c diff colitis". It classically forms pseudomembranes and is often referred to as pseudomembranous colitis, which is its (non-specific) histomorphologic description.
Enterohemorrhagic colitis may be caused by Shiga toxin in Shigella dysenteriae or Shigatoxigenic group of Escherichia coli (STEC), which includes serotype O157:H7 and other enterohemorrhagic E. coli.
Parasitic infections, like those caused by Entamoeba histolytica, can also cause colitis.
Unclassifiable colitides
Indeterminate colitis is the classification for colitis that has features of both Crohn's disease and ulcerative colitis. Indeterminate colitis' behaviour is usually closer to ulcerative colitis than Crohn's disease.
Atypical colitis is a phrase that is occasionally used by physicians for a colitis that does not conform to criteria for accepted types of colitis. It is not an accepted diagnosis per se and, as such, a colitis that cannot be definitively classified.
Treatment
Some people may be admitted into the hospital following the colonoscopy depending on results. It is sometimes necessary to get the patient started on a steroid to speed up the healing of the colon. It may also be necessary to get the patient hydrated from the fluid loss and iron replaced from the loss of blood. Beyond a hospital stay, the patient will be put on a daily medication which they will continuously take since this is a chronic yet manageable condition. The medication can be an anti-inflammatory or an immunosuppressant. There are many different types of medication used and the doctor will prescribe the one they see fit. If the patient doesn't respond, new medications will be tried until there is a good fit. Moreover, several studies recently have found significant relationship between colitis and dairy allergy (including: cow milk, cow milk UHT and casein) suggesting some patients may benefit from an elimination diet.
