 | ||
Probiotics are microorganisms that are believed to provide health benefits when consumed. The term probiotic is currently used to name ingested microorganisms associated with benefits for humans and animals. The term came into more common use after 1980. The introduction of the concept is generally attributed to Nobel laureate Élie Metchnikoff, who postulated that yogurt-consuming Bulgarian peasants lived longer lives because of this custom. He suggested in 1907 that "the dependence of the intestinal microbes on the food makes it possible to adopt measures to modify the flora in our bodies and to replace the harmful microbes by useful microbes". A significant expansion of the potential market for probiotics has led to higher requirements for scientific substantiation of putative benefits conferred by the microorganisms.
Contents
- Etymology
- Definition
- History
- EFSA and FDA scientific reviews
- Research
- Allergies
- Antibiotic associated diarrhea AAD
- Bacterial vaginosis
- Blood pressure
- Cholesterol
- Diarrhea
- Eczema
- Helicobacter pylori
- Immune function and infections
- Inflammation
- Inflammatory bowel disease
- Irritable bowel syndrome
- Lactose intolerance
- Necrotizing enterocolitis
- Urinary tract
- Vitamin production
- Side effects
- Strains
- Labeling
- History and modern products
- Global consumption
- Multiple probiotics
- References
Although there are numerous claimed benefits of using commercial probiotics, such as reduction of gastrointestinal discomfort or strengthening of the immune system, such claims are not backed by scientific evidence.
Probiotics are considered to be generally safe, but they may cause bacteria-host interactions and unwanted side effects in certain cases.
Etymology
Some literature gives it a full Greek etymology, but the term appears to be a composite of the Latin preposition pro ("for") and the Greek adjective βιωτικός (biōtikos), "fit for life, lively", the latter deriving from the noun βίος (bios, "life"). The term contrasts etymologically with the term antibiotic.
Definition
The World Health Organization's (WHO) 2001 definition of probiotics is "live micro-organisms which, when administered in adequate amounts, confer a health benefit on the host". Following this definition, a working group convened by the FAO/WHO in May 2002 issued the “Guidelines for the Evaluation of Probiotics in Food”. This first global effort was further developed in 2010; two expert groups of academic scientists and industry representatives made recommendations for the evaluation and validation of probiotic health claims. The same principles emerged from those groups as the ones expressed in the Guidelines of FAO/WHO in 2002. This definition, although widely adopted, is not acceptable to the European Food Safety Authority because it embeds a health claim which is not measurable.
A consensus definition of the term “probiotics”, based on the available information and scientific evidence, was adopted after a joint Food and Agricultural Organization of the United Nations and World Health Organization expert consultation. In October 2001, this expert consultation defined probiotics as: “live micro-organisms which, when administered in adequate amounts, confer a health benefit on the host”. The FAO/WHO consultation was also a first effort towards the assessment of probiotics efficacy and resulted in May 2002 in a document named “Guidelines for the Evaluation of Probiotics in Food”. This effort was accompanied by local governmental and supra-governmental regulatory bodies requirements to better characterize health claims substantiations.
A group of scientific experts assembled in London, UK, on October 23, 2013, to discuss the scope and appropriate use of the term probiotic. The meeting was motivated by developments in the field since 2001. The panel's conclusions were published in June 2014.
Probiotics have to be alive when administered. One of the concerns throughout the scientific literature resides in the viability and reproducibility on a large scale of the observed results, as well as the viability and stability during use and storage, and finally the ability to survive in stomach acids and then in the intestinal ecosystem. Probiotics must have undergone controlled evaluation to document health benefits in the target host. Only products containing live organisms shown in reproducible human studies to confer a health benefit can actually claim to be a probiotic. The correct definition of health benefit, backed with solid scientific evidence, is a strong element for the proper identification and assessment of the effect of a probiotic. This aspect represents a major challenge for scientific and industrial investigations because several difficulties arise, such as variability in the site for probiotic use (oral, vaginal, intestinal) and mode of application.
The probiotic candidate must be a taxonomically defined microbe or combination of microbes (genus, species, and strain level). It is commonly admitted that most effects of probiotics are strain-specific and cannot be extended to other probiotics of the same genus or species. This calls for a precise identification of the strain, i.e. genotypic and phenotypic characterization of the tested microorganism.
Probiotics must be safe for their intended use. The 2002 FAO/WHO guidelines recommend that, though bacteria may be generally recognized as safe (GRAS), the safety of the potential probiotic should be assessed by the minimum required tests:
In Europe, EFSA has adopted a premarket system for safety assessment of microbial species used in food and feed productions, to set priorities for the need of risk assessment. The assessment is made for a selected group of microorganisms, which if favorable, leads to the “Qualified Presumption of Safety” status.
Finally, probiotics must be supplied in adequate numbers, which may be defined as the number able to trigger the targeted effect on the host. It depends on strain specificity, process, and matrix, as well as the targeted effect. Most of reported benefits demonstrated with the traditional probiotics have been observed after ingestion of a concentration around 107 to 108 probiotic cells per gram, with a serving size around 100 to 200 mg per day.
History
Probiotics have received renewed attention recently from product manufacturers, research studies, and consumers. The history of probiotics can be traced to the first use of cheese and fermented products, that were well known to the Greeks and Romans who recommended their consumption. The fermentation of dairy foods represents one of the oldest techniques for food preservation.
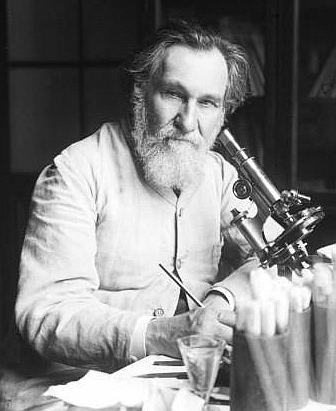
The original modern hypothesis of the positive role played by certain bacteria was first introduced by Russian scientist and Nobel laureate Élie Metchnikoff, who in 1907 suggested that it would be possible to modify the gut flora and to replace harmful microbes with useful microbes. Metchnikoff, at that time a professor at the Pasteur Institute in Paris, proposed the hypothesis that the aging process results from the activity of putrefactive (proteolytic) microbes producing toxic substances in the large bowel. Proteolytic bacteria such as clostridia, which are part of the normal gut flora, produce toxic substances including phenols, indols, and ammonia from the digestion of proteins. According to Metchnikoff, these compounds were responsible for what he called "intestinal autointoxication", which would cause the physical changes associated with old age.
It was at that time known that milk fermented with lactic-acid bacteria inhibits the growth of proteolytic bacteria because of the low pH produced by the fermentation of lactose. Metchnikoff had also observed that certain rural populations in Europe, for example in Bulgaria and the Russian steppes, who lived largely on milk fermented by lactic-acid bacteria were exceptionally long lived. Based on these observations, Metchnikoff proposed that consumption of fermented milk would "seed" the intestine with harmless lactic-acid bacteria and decrease the intestinal pH, and that this would suppress the growth of proteolytic bacteria. Metchnikoff himself introduced in his diet sour milk fermented with the bacteria he called "Bulgarian Bacillus" and believed his health benefited. Friends in Paris soon followed his example and physicians began prescribing the sour-milk diet for their patients.
Bifidobacteria were first isolated from a breast-fed infant by Henry Tissier, who also worked at the Pasteur Institute. The isolated bacterium named Bacillus bifidus communis was later renamed to the genus Bifidobacterium. Tissier found that bifidobacteria are dominant in the gut flora of breast-fed babies and he observed clinical benefits from treating diarrhea in infants with bifidobacteria. The claimed effect was bifidobacterial displacement of proteolytic bacteria causing the disease.
During an outbreak of shigellosis in 1917, German professor Alfred Nissle isolated a strain of Escherichia coli from the feces of a soldier who was not affected by the disease. Methods of treating infectious diseases were needed at that time when antibiotics were not yet available, and Nissle used the E. coli Nissle 1917 strain in acute gastrointestinal infectious salmonellosis and shigellosis.
In 1920, Rettger and Cheplin reported that Metchnikoff's "Bulgarian Bacillus", later called Lactobacillus delbrueckii subsp. bulgaricus, could not live in the human intestine. They conducted experiments involving rats and humans volunteers, by feeding them with Lactobacillus acidophilus. They observed changes in composition of fecal microbiota, which they described as “transformation of the intestinal flora”. Rettger further explored the possibilities of L. acidophilus and reasoned that bacteria originating from the gut were more likely to produce the desired effect in this environment. In 1935, certain strains of L. acidophilus were found to be very active when implanted in the human digestive tract. Trials were carried out using this organism, and encouraging results were obtained, especially in the relief of chronic constipation.
Contrasting antibiotics, probiotics were defined as microbially derived factors that stimulate the growth of other microorganisms. In 1989, Roy Fuller suggested a definition of probiotics that has been widely used: "A live microbial feed supplement which beneficially affects the host animal by improving its intestinal microbial balance". Fuller's definition emphasizes the requirement of viability for probiotics and introduces the aspect of a beneficial effect on the host.
The term "probiotic" originally referred to microorganisms that have effects on other microorganisms. The conception of probiotics involved the notion that substances secreted by one microorganism stimulated the growth of another microorganism. The term was used again to describe tissue extracts which stimulated microbial growth. The term probiotics was taken up by Parker, who defined the concept as, “organisms and substances that have a beneficial effect on the host animal by contributing to its intestinal microbial balance”. Later, the definition was greatly improved by Fuller, whose explanation was very close to the definition used today. Fuller 89 described probiotics as a "live microbial feed supplement which beneficially affects the host animal by improving its intestinal microbial balance". He stressed two important facts of probiotics: the viable nature of probiotics and the capacity to help with intestinal balance.
In the following decades, intestinal lactic acid bacterial species with alleged health beneficial properties have been introduced as probiotics, including Lactobacillus rhamnosus, Lactobacillus casei, and Lactobacillus johnsonii.
EFSA and FDA scientific reviews
The European Food Safety Authority has rejected all petitions by commercial manufacturers for health claims on probiotic products in Europe due to insufficient research and thus inconclusive proof of effectiveness. Occurring over many years, the scientific reviews established that a cause-and-effect relationship had not been sufficiently proven in the products submitted.
In the United States where food product labeling requires language approval by the FDA, probiotic manufacturers have received warning letters of impending legal actions for using exaggerated claims of health benefits not supported by clinical evidence of efficacy.
Research
Probiotics have been the subject of research to see whether the health claims made for them have any supporting evidence. Overall scientific demonstration of probiotic effects requires defining a healthy microbiota and interactions between microbiota and host, and the difficulty to characterize probiotic effectiveness in health and disease. Recent developments of high-throughput sequencing technology and the consequent progresses of metagenomics represent a new approach for the future of probiotics research.
Studies are examining whether probiotics affect mechanisms of intestinal inflammation, diarrhea, or urogenital infections. Through 2012, however, in all cases proposed as health claims to the European Food Safety Authority, the scientific evidence remains insufficient to prove a cause-and-effect relationship between consumption of probiotic products and any health benefit.
Research into the potential health effects of supplemental probiotics has included the molecular biology and genomics of Lactobacillus in immune function, cancer, and antibiotic-associated diarrhea, travellers' diarrhea, pediatric diarrhea, inflammatory bowel disease, and irritable bowel syndrome. Testing of a probiotic applies to a specific strain under study. The scientific community cautions against extrapolating an effect from a tested strain to an untested strain.
Although research does suggest that the relationship between gut flora and humans is a mutualistic relationship, very little evidence supports claims that probiotic dietary supplements have any health benefits. Improved health through gut flora modulation appears to be directly related to long-term dietary changes.
Claims that some lactobacilli may contribute to weight gain in some humans remain controversial.
Allergies
Probiotics are ineffective in preventing allergies in children, with the possible exception of eczema.
Antibiotic-associated diarrhea (AAD)
Antibiotics are a common treatment for children, and 20% of antibiotic-treated children develop diarrhea. Antibiotic-associated diarrhea results from an imbalance in the colonic microbiota caused by antibiotic therapy. Microbiota alteration changes carbohydrate metabolism, with decreased short-chain fatty acid absorption and osmotic diarrhea as a result. A review assessing the work of 16 different studies representing the evaluation of more than 3,400 patients concluded that the evidence gathered suggested a protective effect of some probiotics in this condition. In adults, some probiotics showed a beneficial role in reducing the occurrence of AAD.
Probiotic treatment might reduce the incidence and severity of AAD as indicated in several meta-analyses. For example, treatment with probiotic formulations including L. rhamnosus may reduce the risk of AAD, improve stool consistency during antibiotic therapy, and enhance the immune response after vaccination.
The potential efficacy of probiotic AAD prevention is dependent on the probiotic strain(s) used and on the dosage. A Cochrane Collaboration systematic review, in which 16 randomized clinical trials (n=3432 participants) were analyzed, concluded that treatments with less than 7009500000000000000♠5×109 CFUs/day did not show a significant decrease of AAD. However, patients treated with ≥7009500000000000000♠5×109 CFUs/day (including L. rhamnosus and Saccharomyces boulardii) had 60% lower relative risk (95%CI: 44–71%) of experiencing AAD than untreated patients.
Bacterial vaginosis
Probiotic treatment of bacterial vaginosis is the application or ingestion of bacterial species found in the healthy vagina to cure the infection of bacteria causing bacterial vaginosis. This treatment is based on the observation that 70% of healthy females have a group of bacteria in the genus Lactobacillus that dominate the population of organisms in the vagina. Currently, the success of such treatment has been mixed since the use of probiotics to restore healthy populations of Lactobacillus has not been standardized. Often, standard antibiotic treatment is used at the same time that probiotics are being tested. In addition, some groups of women respond to treatment based upon ethnicity, age, number of sexual partners, pregnancy, and the pathogens causing bacterial vaginosis. In 2013, researchers found that administration of hydrogen peroxide producing strains, such as L. acidophilus and L. rhamnosus, were able to normalize vaginal pH and rebalance vaginal flora, preventing and alleviating bacterial vaginosis.
Blood pressure
The consumption of probiotics may modestly help to control high blood pressure.
Cholesterol
Preliminary human and animal studies have demonstrated the efficacy of some strains of lactic acid bacteria (LAB) for reducing serum cholesterol levels, presumably by breaking down bile in the gut, thus inhibiting its reabsorption (where it enters the blood as cholesterol).
A meta-analysis that included five double-blind trials examining the short-term (2–8 weeks) effects of a yogurt with probiotic strains on serum cholesterol levels found a minor change of 8.5 mg/dL (0.22 mmol/L) (4% decrease) in total cholesterol concentration, and a decrease of 7.7 mg/dL (0.2 mmol/L) (5% decrease) in serum LDL concentration.
A slightly longer study evaluating the effect of a yogurt with probiotic strains on 29 subjects over six months found no statistically significant differences in total serum cholesterol or LDL values. However, the study did note a significant increase in serum HDL from, 50 to 62 mg/dL (1.28 to 1.6 mmol/L) following treatment. This corresponds to a possible improvement of LDL/HDL ratio.
Studies specifically on hyperlipidemic subjects are still needed.
Diarrhea
Some probiotics are suggested as a possible treatment for various forms of gastroenteritis, and a Cochrane Collaboration meta-analysis on the use of probiotics to treat acute infectious diarrhea based on a comprehensive review of medical literature through 2010 (35 relevant studies, >4500 participants) reported that use of any of the various tested probiotic formulations appeared to reduce the duration of diarrhea by a mean of 25 hours (vs. control groups, 95% confidence interval, 16–34 hours), also noting, however, that "the differences between the studies may be related to other unmeasured and unexplored environmental and host factors" and that further research was needed to confirm reported benefits.
Eczema
Probiotics are commonly given to breast-feeding mothers and their young children to prevent eczema, but some doubt exists over the strength of evidence supporting this practice.
Helicobacter pylori
Some strains of lactic acid bacteria may affect Helicobacter pylori infections (which may cause peptic ulcers) in adults when used in combination with standard medical treatments, but no standard in medical practice or regulatory approval exists for such treatment.
Immune function and infections
Some strains of lactic acid bacteria (LAB) may affect pathogens by means of competitive inhibition (i.e., by competing for growth) and some evidence suggests they may improve immune function by increasing the number of IgA-producing plasma cells and increasing or improving phagocytosis, as well as increasing the proportion of T lymphocytes and natural killer cells. Clinical trials have demonstrated that probiotics may decrease the incidence of respiratory-tract infections and dental caries in children. LAB products might aid in the treatment of acute diarrhea, and possibly affect rotavirus infections in children and travelers' diarrhea in adults, but no products are approved for such indications.
Inflammation
Some strains of LAB may modulate inflammatory and hypersensitivity responses, an observation thought to be at least in part due to the regulation of cytokine function. Clinical studies are assessing whether they can prevent recurrences of inflammatory bowel disease in adults, as well as affect milk allergies. How probiotics may influence the immune system remains unclear.
Inflammatory bowel disease
Probiotics are being studied for their potential to influence inflammatory bowel disease. There is some evidence to support their use in conjunction with standard medications in treating ulcerative colitis and no evidence of their efficacy in treating Crohn's disease.
A live formulation of lyophilized Bifidobacterium breve, Bifidobacterium longum, Bifidobacterium infantis, Lactobacillus acidophilus, Lactobacillus plantarum, Lactobacillus paracasei, Lactobacillus bulgaricus, and Streptococcus thermophilus (VSL#3) has shown effectiveness in the small clinical trials, some of which were not randomized nor double-blinded, that had been done as of 2015; more high quality clinical trials are needed to determine safety and effectiveness.
Irritable bowel syndrome
Probiotics are under study for their potential to affect irritable bowel syndrome, although uncertainty remains around which type of probiotic works best, and around the size of possible effect.
Lactose intolerance
Ingestion of certain active strains may help lactose-intolerant individuals tolerate more lactose than they would otherwise have tolerated.
Necrotizing enterocolitis
Several clinical studies provide evidence for the potential of probiotics to lower the risk of necrotizing enterocolitis and mortality in premature infants. One meta-analysis indicated that probiotics reduce these risks by more than 50% compared with controls.
Urinary tract
There is no good evidence that probiotics are of benefit in the management of infection or inflammation of the urinary tract.
Vitamin production
Probiotic treatment has been studied as a means of addressing disorders associated with vitamin deficiencies including those of vitamin K, folic acid, and vitamin B12.
Side effects
The manipulation of the gut microbiota is complex and may cause bacteria-host interactions. Although probiotics are considered to be safe, there are concerns about their safety in certain cases. Some people, such as those with immunodeficiency, short bowel syndrome, central venous catheters, cardiac valve disease and premature infants, may be at higher risk for adverse events. In severely ill people with inflammatory bowel disease there is a risk of the passage of viable bacteria from the gastrointestinal tract to the internal organs (bacterial translocation) as a consequence of bacteremia, which can cause adverse health consequences. Rarely, consumption of probiotics by children with lowered immune system function or who are already critically ill may result in bacteremia or fungemia (i.e., bacteria or fungi in the blood), which can lead to sepsis, a potentially fatal disease.
Although it has been suggested that Lactobacillus contributes to obesity in humans, no evidence of this relationship has been found.
Strains
Live probiotic cultures are available in fermented dairy products and probiotic fortified foods. However, tablets, capsules, powders, and sachets containing the bacteria in freeze-dried form are also available. Probiotics taken orally can be destroyed by the acidic conditions of the stomach. A number of microencapsulation techniques are being developed to address this problem.
Only preliminary evidence exists for most probiotic health claims. Even for the most studied strains, few have been sufficiently developed in basic and clinical research to warrant approval for health claim status by a regulatory agency such as the Food and Drug Administration or European Food Safety Authority, and as of 2010, no claims have been approved by those two agencies. Some experts are skeptical about the efficacy of different strains and believe not all subjects will benefit from the use of probiotics.
Some fermented products are reported to contain lactic acid bacteria, including pickled vegetables, tempeh, miso, kefir, buttermilk or karnemelk, kimchi, pao cai, sauerkraut, and soy sauce.
Labeling
The US National Yogurt Association gives a Live & Active Cultures Seal to refrigerated yogurt products which contain 100 million cultures per gram or frozen yogurt products containing 10 million cultures per gram at the time of manufacture. In 2002, the US Food and Drug Administration (FDA) and World Health Organization recommended that “the minimum viable numbers of each probiotic strain at the end of the shelf-life” be reported on labeling, but most companies that give a number report the viable cell count at the date of manufacture, a number probably much higher than existing at the moment of consumption. Because of variability in storage conditions and time before eating, it is difficult to tell exactly how much active culture remains at the time of consumption.
Due to these ambiguities, the European Commission placed a ban on putting the word “probiotic” on the packaging of products because such labeling misleads consumers to believe a health benefit is provided by the product when no scientific proof exists to demonstrate that health effect.
In the United States, the FDA has issued warning letters to various manufacturers of probiotic products whose labels claim unproven nutritional benefits or anti-disease activity.
History and modern products
The first commercially sold dairy-based probiotic was Yakult, a fermented milk with added Lactobacillus casei Shirota, in 1935. Since then, many more probiotic foods have come on the market, mostly in the form of dairy products. Recently, nondairy and unfermented probiotics have been produced, including breakfast cereal and snack bars, whereas other probiotic products include kefir, yogurt, kombucha, kimchi, sauerkraut and other fermented foods and beverages.
Global consumption
Sales of probiotic products have a rising trend from 2010 to 2014, increasing globally by 35% from US$23.1 billion to $31.3 billion. Some regions have increased their use by even more than the average, including Eastern Europe (67%), Asia Pacific (67%), and Latin America (47%), comprising nearly half of probiotics sold globally in 2014. By geographic region, the leading consumers of probiotics in 2014 were Western Europe ($8.3 billion), Asia Pacific ($7 billion), Japan ($5.4 billion), Latin America ($4.8 billion), North America ($3.5 billion), and Eastern Europe ($2.3 billion).
Multiple probiotics
Preliminary research is evaluating the potential physiological effects of multiple probiotic strains, as opposed to a single strain. As the human gut may contain several hundred microbial species, one theory indicates that this diverse environment may benefit from consuming multiple probiotic strains, an effect that remains scientifically unconfirmed.
