 | ||
Biological therapy refers to the use of medication that is tailored to specifically target an immune or genetic mediator of disease. Even for diseases of unknown cause, molecules that are involved in the disease process have been identified, and can be targeted for biological therapy; many of these molecules, which are mainly cytokines, are directly involved in the immune system. Biological therapy has found a niche in the management of cancer, autoimmune diseases, and diseases of unknown cause that result in symptoms due to immune related mechanisms.
Contents
- Rationale for biological therapy
- Infliximab
- Other monoclonal antibodies
- Side effects and concerns
- Research
- References
Inflammatory bowel disease, or IBD, is a collection of systemic diseases involving inflammation of the gastrointestinal tract. IBD includes two (or three) diseases of unknown causation: ulcerative colitis, which affects only the large bowel; Crohn's disease, which can affect the entire gastrointestinal tract; and, indeterminate colitis, which consists of large bowel inflammation that shows elements of both Crohn's disease and ulcerative colitis.
Although the causes of these diseases are unknown, genetic, environmental, immune and other mechanisms have been proposed. Of these, the immune system plays a large role in the development of symptoms. Given this, a variety of biological therapies have been developed for the treatment of these diseases. These have changed the way physicians treat Crohn's disease and ulcerative colitis.
Rationale for biological therapy
Prior to the development of biological therapy as a modality to treat IBD, other medications that modulate the immune system—including 5-aminosalicylates, steroids, azathioprine, and other immunosuppressants—were primarily used in treatment. Patients with Crohn's disease that developed complications, including fistulae (= abnormal connections to the bowel) were treated with surgery. Patients with ulcerative colitis who do not respond to medications are still treated with colectomy (= removal of the colon).
However, basic science research showed that there were many cytokines that were elevated in both Crohn's disease and ulcerative colitis. Crohn's disease cytokines, are of the type 1 (Th1) cytokines which include TNF-α, interleukin-2, and interferon γ. Ulcerative colitis was less conclusively linked to the production of Th2 cytokines.
Infliximab
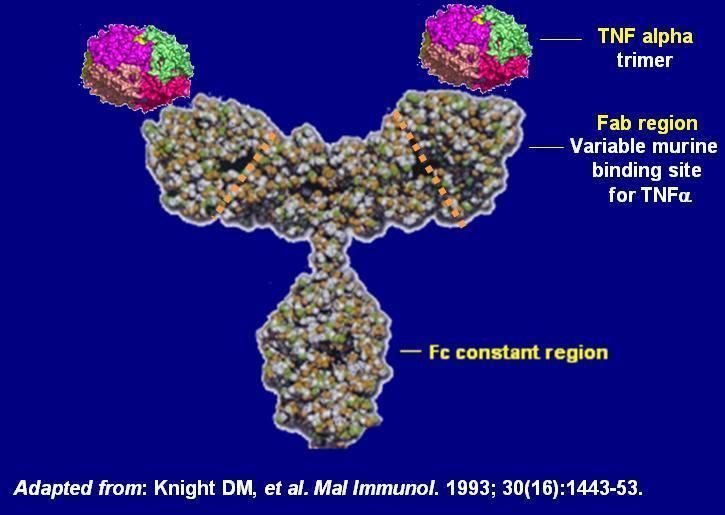
The monoclonal antibody infliximab is a mouse-human chimeric antibody to TNF-α. It first was used in the treatment of rheumatoid arthritis, and was the first biological agent used in the treatment of IBD. It is also used in the treatment of psoriasis and ankylosing spondylitis. Infliximab has shown significant success in treating Crohn's disease.
Other monoclonal antibodies
Other biological therapy agents and monoclonal antibodies have not showed as much efficacy in the treatment of IBD. These include etanercept (which is the soluble receptor for TNF. Adalimumab (which is a humanized recombinant antibody to TNF) showed effectiveness in patients with moderate-to-severe Crohn's disease, but less than that of infliximab. It however conveys an advantage in that it is given by subcutaneous injection as opposed to infliximab, which is given by intravenous infusion.
In 2005, two other recombinant medications were reported to have benefit in moderate to severe Crohn's disease. Certolizumab is a Fab fragment of a humanized anti-TNF alpha monoclonal antibody that is attached to polyethylene glycol to increase its half-life in circulation. It was found to have efficacy over placebo medications for 10 weeks in the treatment of moderate to severe Crohn's disease in one large trial. Natalizumab is an anti-integrin monoclonal antibody that shown utility as induction and maintenance treatment for moderate to severe Crohn's disease. However, it has been associated with progressive multifocal leukoencephalopathy, a usually fatal viral infection of the brain, that may limit its use.
Side effects and concerns
There have been concerns about the side effects of monoclonal antibodies, and specifically of infliximab, but these are rare. Early side effects include the risk of allergic reactions (including anaphylaxis which may be life-threatening), and reactions to the infusion. These are often treated with medications given before treatment. Infliximab also carries a risk of worsening infection, and can cause reactivation of old infections, like tuberculosis. Over time, there is the risk of serum sickness, which is a delayed hypersensitivity response to the medication. Later complications may include multiple sclerosis and lymphoma. Finally, the medication is quite expensive, with treatment costs ranging from US$3000 to $8000 per infusion.
Loss of response to infliximab over time is a concern, due to the development of antibodies to infliximab (termed human anti-chimeric antibodies, or HACA). This can be reduced by concurrent treatment with other immunosuppressant medications (including azathioprine and methotrexate), by maintaining a regular infusion schedule, and by giving patients a pre-treatment dose of steroid medication.
Biologic agents may promote developing malignancies due to they act on the immune system.
Research
Gram positive bacteria present in the lumen could be associated with extending the time of relapse for ulcerative colitis.
