Specialty Gynecology ICD-9-CM 617.0 DiseasesDB 4269 | ICD-10 N80 OMIM 131200 MedlinePlus 000915 | |
 | ||
Endometriosis is a condition in which tissue that normally grows inside the uterus (endometrium) grows outside it. Most often this is on the ovaries, fallopian tubes, and tissue around the uterus and ovaries; however, in rare cases it may also occur in other parts of the body. The main symptoms are pelvic pain and infertility. Nearly half of those affected have chronic pelvic pain, while in 70% pain occurs during menstruation. Pain during sex is also common. Infertility occurs in up to half of women affected. Less common symptoms include urinary or bowel symptoms. About 25% of women have no symptoms. Endometriosis can have both social and psychological effects.
Contents
- Signs and symptoms
- Pelvic pain
- Infertility
- Other
- Genetics
- Environmental toxins
- Pathophysiology
- Formation
- Retrograde menstruation theory
- Other theories
- Localization
- Diagnosis
- Laparoscopy
- Staging
- Markers
- Histopathology
- Pain quantification
- Prevention
- Management
- Surgery
- Hormones
- Other medication
- Comparison of interventions
- Treatment of infertility
- Prognosis
- Complications
- Epidemiology
- History
- Society and culture
- References
The cause is not entirely clear. Risk factors include having a family history of the condition. The areas of endometriosis bleed each month, resulting in inflammation and scarring. The growths due to endometriosis are not cancer. Diagnosis is usually based on symptoms in combination with medical imaging. Biopsy is the most sure method of diagnosis. Other causes of similar symptoms include pelvic inflammatory disease, irritable bowel syndrome, interstitial cystitis, and fibromyalgia.
Tentative evidence suggests that the use of combined oral contraceptives reduces the risk of endometriosis. Exercise and avoiding large amounts of alcohol may also be preventive. There is no cure for endometriosis, but a number of treatments may improve symptoms. This may include pain medication, hormonal treatments, or surgery. The recommended pain medication is usually an NSAID such as naproxen. Taking the active component of the birth control pill continuously or using an intrauterine device with progestogen may also be useful. Gonadotropin-releasing hormone agonist may improve the ability of those who are infertile to get pregnant. Surgical removal of endometriosis may be used to treat those whose symptoms are not manageable with other treatments.
Endometriosis is estimated to occur in roughly 6–10% of women. It is most common in those in their thirties and forties; however, can begin in girls as early as 8 years old. It results in few deaths with this being estimated at 200 globally in 2013. Endometriosis was first determined to be a separate condition in the 1920s. Before that time endometriosis and adenomyosis were considered together. It is unclear who first described the disease.
Signs and symptoms
Although 20–25% of women with endometriosis have no symptoms, pain and infertility are common signs.
Pelvic pain
A major symptom of endometriosis is recurring pelvic pain. The pain can range from mild to severe cramping or stabbing pain that occurs on both sides of the pelvis, in the lower back and rectal area, and even down the legs. The amount of pain a woman feels correlates poorly with the extent or stage (1 through 4) of endometriosis, with some women having little or no pain despite having extensive endometriosis or endometriosis with scarring, while other women may have severe pain even though they have only a few small areas of endometriosis. Symptoms of endometriosis-related pain may include:
Throbbing, gnawing, and dragging pain to the legs are reported more commonly by women with endometriosis. Compared with women with superficial endometriosis, those with deep disease appear to be more likely to report shooting rectal pain and a sense of their insides being pulled down. Individual pain areas and pain intensity appears to be unrelated to the surgical diagnosis, and the area of pain unrelated to area of endometriosis.
Endometriosis lesions react to hormonal stimulation and may "bleed" at the time of menstruation. The blood accumulates locally, causes swelling, and triggers inflammatory responses with the activation of cytokines. This process may cause pain. Pain can also occur from adhesions (internal scar tissue) binding internal organs to each other, causing organ dislocation. Fallopian tubes, ovaries, the uterus, the bowels, and the bladder can be bound together in ways that are painful on a daily basis, not just during menstrual periods.
Also, endometriotic lesions can develop their own nerve supply, thereby creating a direct and two-way interaction between lesions and the central nervous system, potentially producing a variety of individual differences in pain that can, in some women, become independent of the disease itself. Nerve fibres and blood vessels are thought to grow into endometriosis lesions by a process known as Neuroangiogenesis.
Infertility
Many women with infertility may have endometriosis. Among women with endometriosis, up to half may experience infertility.
Other
Other symptoms include diarrhea or constipation, chronic fatigue, nausea and vomiting, headaches, low-grade fevers, heavy and/or irregular periods, and hypoglycemia.
In addition to pain during menstruation, the pain of endometriosis can occur at other times of the month. There can be a pain with ovulation, pain associated with adhesions, pain caused by inflammation in the pelvic cavity, pain during bowel movements and urination, during general bodily movement like exercise, pain from standing or walking, and pain with intercourse. The most severe pain is typically associated with menstruation. Pain can also start a week before a menstrual period, during and even a week after a menstrual period, or it can be constant. The pain can be debilitating and the emotional stress can take a toll.
There is an association between endometriosis and certain types of cancers, notably some types of ovarian cancer, non-Hodgkin's lymphoma and brain cancer. Endometriosis is unrelated to endometrial cancer.
Genetics
Genetic predisposition plays a role in endometriosis. Daughters or sisters of women with endometriosis are at higher risk of developing endometriosis themselves; low progesterone levels may be genetic, and may contribute to a hormone imbalance. There is an about six-fold increased incidence in women with an affected first-degree relative.
It has been proposed that endometriosis results from a series of multiple hits within target genes, in a mechanism similar to the development of cancer. In this case, the initial mutation may be either somatic or heritable.
Individual genomic changes (found by genotyping including genome-wide association studies) that have been associated with endometriosis include:
In addition, there is a weaker association with changes in the fibronectin gene as well as in the 2p14 region of chromosome 2.
In addition, there are many findings of altered gene expression and epigenetics, but both of these can also be a secondary result of, for example, environmental factors and altered metabolism. Examples of altered gene expression include that of miRNAs.
Environmental toxins
Several studies have investigated the potential link between exposure to dioxins and endometriosis, but the evidence is equivocal and potential mechanisms are poorly understood. A 2004 review of studies of dioxin and endometriosis concluded that "the human data supporting the dioxin-endometriosis association are scanty and conflicting", and a 2009 follow-up review also found that there was "insufficient evidence" in support of a link between dioxin exposure and women developing endometriosis. A 2008 review concluded that more work was needed, stating that "although preliminary work suggests a potential involvement of exposure to dioxins in the pathogenesis of endometriosis, much work remains to clearly define cause and effect and to understand the potential mechanism of toxicity".
Pathophysiology
While the exact cause of endometriosis remains unknown, many theories have been presented to better understand and explain its development. These concepts do not necessarily exclude each other. The pathophysiology of endometriosis is likely to be multifactorial and to involve an interplay between several factors.
Formation
The main theories for the formation of the ectopic endometrium are retrograde menstruation, müllerianosis, coelomic metaplasia and transplantation, each further described below.
Retrograde menstruation theory
The theory of retrograde menstruation (also called the implantation theory or transplantation theory) is the most widely accepted theory for the formation of ectopic endometrium in endometriosis. It suggests that during a woman's menstrual flow, some of the endometrial debris exits the uterus through the fallopian tubes and attaches itself to the peritoneal surface (the lining of the abdominal cavity) where it can proceed to invade the tissue as endometriosis.
Retrograde menstruation alone is not able to explain all instances of endometriosis, and additional factors such as genetic or immune differences need to be invoked to account for the fact that many women with retrograde menstruation do not have endometriosis. Researchers are investigating the possibility that the immune system may not be able to cope with the cyclic onslaught of retrograde menstrual fluid. In this context there is interest in studying the relationship of endometriosis to autoimmune disease, allergic reactions, and the impact of toxic materials. It is still unclear what, if any, causal relationship exists between toxic materials, autoimmune disease, and endometriosis. There are immune system changes in women with endometriosis, such as an increase macrophage-derived secretion products, but it is unknown if these are contributing to the disorder or are reactions from it.
In addition, at least one study found that endometriotic lesions differ in their biochemistry from artificially transplanted ectopic tissue. This is likely because the cells that give rise to endometriosis are a side population of cells. Similarly, there are changes in for example the mesothelium of the peritoneum in women with endometriosis, such as loss of tight junctions, but it is unknown if these are causes or effects of the disorder.
In rare cases where imperforate hymen does not resolve itself prior to the first menstrual cycle and goes undetected, blood and endometrium are trapped within the uterus of the woman until such time as the problem is resolved by surgical incision. Many health care practitioners never encounter this defect, and due to the flu-like symptoms it is often misdiagnosed or overlooked until multiple menstrual cycles have passed. By the time a correct diagnosis has been made, endometrium and other fluids have filled the uterus and fallopian tubes with results similar to retrograde menstruation resulting in endometriosis. The initial stage of endometriosis may vary based on the time elapsed between onset and surgical procedure.
The theory of retrograde menstruation as a cause of endometriosis was first proposed by John A. Sampson.
Other theories
Localization
Most endometriosis is found on these structures in the pelvic cavity:
Rectovaginal or bowel endometriosis affects approximately 5-12% of women with endometriosis, and can cause severe pain with bowel movements.
Endometriosis may spread to the cervix and vagina or to sites of a surgical abdominal incision, known as "scar endometriosis." Risk factors for scar endometriosis include previous abdominal surgeries, such as a hysterotomy or cesarean section, or ectopic pregnancies, salpingostomy puerperal sterilization, laparoscopy, amniocentesis, appendectomy, episiotomy, vaginal hysterectomies, and hernia repair.
Endometriosis may also present with skin lesions in cutaneous endometriosis.
Less commonly lesions can be found on the diaphragm. Diaphragmatic endometriosis is rare, almost always on the right hemidiaphragm, and may inflict the cyclic pain of the right shoulder just before and during a menstrual period. Rarely, endometriosis can be extraperitoneal and is found in the lungs and CNS.
Diagnosis
A health history and a physical examination can lead the health care practitioner to suspect endometriosis. Although doctors can often feel the endometrial growths during a pelvic exam, and these symptoms may be signs of endometriosis, diagnosis cannot be confirmed by exam only. Use of pelvic ultrasound may identify large endometriotic cysts (called endometriomas). However, smaller endometriosis implants cannot be visualized with ultrasound technique.
Laparoscopy
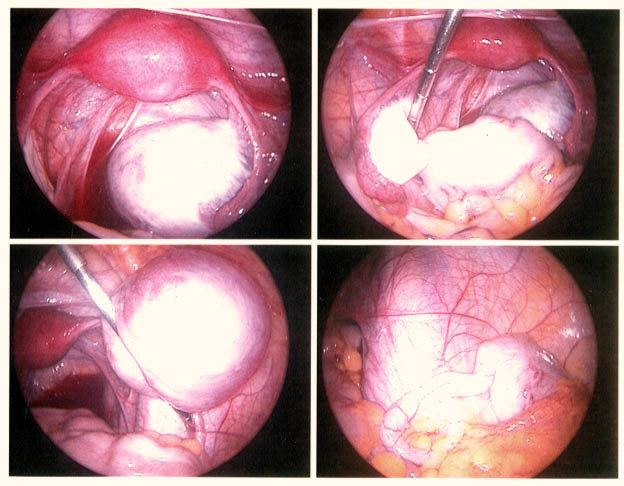
Laparoscopy, a surgical procedure where a camera is used to look inside the abdominal cavity, is the only way to officially diagnose endometriosis as it permits lesion visualization unless the lesion is visible externally, e.g. an endometriotic nodule in the vagina. If the growths are not visible, a biopsy may be taken to determine the diagnosis. Surgery for diagnoses also allows for surgical treatment of endometriosis at the same time.
To the eye, lesions can appear dark blue, powder-burn black, red, white, yellow, brown or non-pigmented. Lesions vary in size. Some within the pelvis walls may not be visible, as normal-appearing peritoneum of infertile women reveals endometriosis on biopsy in 6–13% of cases. Early endometriosis typically occurs on the surfaces of organs in the pelvic and intra-abdominal areas. Health care providers may call areas of endometriosis by different names, such as implants, lesions, or nodules. Larger lesions may be seen within the ovaries as endometriomas or "chocolate cysts", "chocolate" because they contain a thick brownish fluid, mostly old blood.
Frequently during diagnostic laparoscopy, no lesions are found in women with chronic pelvic pain, a symptom common to other disorders including adenomyosis, pelvic adhesions, pelvic inflammatory disease, congenital anomalies of the reproductive tract, and ovarian or tubal masses.
Staging
Surgically, endometriosis can be staged I–IV by the revised classification of the American Society of Reproductive Medicine from 1997. The process is a complex point system that assesses lesions and adhesions in the pelvic organs, but it is important to note staging assesses physical disease only, not the level of pain or infertility. A person with Stage I endometriosis may have a little disease and severe pain, while a person with Stage IV endometriosis may have severe disease and no pain or vice versa. In principle the various stages show these findings:
Markers
An area of research is the search for endometriosis markers.
In 2010 essentially all proposed biomarkers for endometriosis were of unclear medical use, although some appear to be promising. The one biomarker that has been in use over the last 20 years is CA-125. A 2016 review found that in those with symptoms of endometriosis and once ovarian cancer has been ruled out, a positive CA-125 may confirm the diagnosis. Its performance in ruling out endometriosis; however, is low. CA-125 levels appear to fall during endometriosis treatment, but has not shown a correlation with disease response.
Another review in 2011 identified several putative biomarkers upon biopsy, including findings of small sensory nerve fibers or defectively expressed β3 integrin subunit. It has been postulated a future diagnostic tool for endometriosis will consist of a panel of several specific and sensitive biomarkers, including both substance concentrations and genetic predisposition.
Histopathology
Typical endometriotic lesions show histopathologic features similar to endometrium, namely endometrial stroma, endometrial epithelium, and glands that respond to hormonal stimuli. Older lesions may display no glands but hemosiderin deposits (see photomicrograph on right) as residual.
Immunohistochemistry has been found to be useful in diagnosing endometriosis as stromal cells have a peculiar surface antigen, CD10, thus allowing the pathologist go straight to a staining area and hence confirm the presence of stromal cells and sometimes glandular tissue is thus identified that was missed on routine H&E staining.
Pain quantification
The most common pain scale for quantification of endometriosis-related pain is the visual analogue scale (VAS); VAS and numerical rating scale (NRS) were the best adapted pain scales for pain measurement in endometriosis. For research purposes, and for more detailed pain measurement in clinical practice, VAS or NRS for each type of typical pain related to endometriosis (dysmenorrhea, deep dyspareunia and non-menstrual chronic pelvic pain), combined with the clinical global impression (CGI) and a quality of life scale, are used.
Prevention
Limited evidence indicates that the use of combined oral contraceptives is associated with a reduced risk of endometriosis.
Management
While there is no cure for endometriosis, there are two types of interventions; treatment of pain and treatment of endometriosis-associated infertility. In many women menopause (natural or surgical) will abate the process. In women in the reproductive years, endometriosis is merely managed: the goal is to provide pain relief, to restrict progression of the process, and to restore or preserve fertility where needed. In younger women, surgical treatment attempts to remove endometrial tissue and preserve the ovaries without damaging normal tissue.
In general, the diagnosis of endometriosis is confirmed during surgery, at which time ablative steps can be taken. Further steps depend on circumstances: a woman without infertility can be managed with hormonal medication that suppresses the natural cycle and pain medication, while an infertile woman may be treated expectantly after surgery, with fertility medication, or with IVF. As to the surgical procedure, ablation (or fulguration) of endometriosis (burning and vaporizing the lesions with an electric device) has shown a high rate of short-term recurrence after the procedure. The best surgical procedure with much less rate of short-term recurrence is to excise (cut and remove) the lesions completely.
Surgery
Conservative treatment consists of the excision of the endometrium, adhesions, resection of endometriomas, and restoration of normal pelvic anatomy as much as is possible. Endometrioma on the ovary of any significant size (Approx. 2 cm +) -sometimes misdiagnosed as ovarian cysts- must be removed surgically because hormonal treatment alone will not remove the full endometrioma cyst, which can progress to acute pain from the rupturing of the cyst and internal bleeding. Laparoscopy, besides being used for diagnosis, can also be used to perform surgery. It's considered a "minimally invasive" surgery because the surgeon makes very small openings (incisions) at (or around) the belly button and lower portion of the belly. A thin telescope-like instrument (the laparoscope) is placed through one incision, which allows the doctor to look for endometriosis using a small camera attached to the laparoscope. Small instruments are inserted through the incisions to remove the endometriosis tissue and adhesions. Because the incisions are very small, there will only be small scars on the skin after the procedure, and all endometriosis can be removed, and women recover from surgery quicker and have a lower risk of adhesions.
55% to 100% of women develop adhesions following pelvic surgery, which can result in infertility, chronic abdominal and pelvic pain, and difficult reoperative surgery. Trehan's temporary ovarian suspension, a technique in which the ovaries are suspended for a week after surgery may be used to reduce the incidence of adhesions after endometriosis surgery.
Conservative treatment involves excision of endometriosis while preserving the ovaries and uterus, very important for women wishing to conceive, but may increase the risk of recurrence.
Endometriosis recurrence following conservative surgery is estimated as 21.5% at 2 years and 40-50% at 5 years.
A hysterectomy (removal of the uterus) can be used to treat endometriosis in women who do not wish to conceive. However, this should only be done when combined with removal of the endometriosis by excision, as if endometriosis is not also removed at the time of hysterectomy, pain may persist.
For women with extreme pain, a presacral neurectomy may be very rarely performed where the nerves to the uterus are cut. However, this technique is almost never used due to the high incidence of associated complications including presacral hematoma and irreversible problems with urination and constipation.
Hormones
Other medication
The overall effectiveness of manual physical therapy to treat endometriosis has not yet been identified. There is no evidence to support nutritional therapy as effective.
Comparison of interventions
Medicinal and surgical interventions produce roughly equivalent pain-relief benefits. Recurrence of pain was found to be 44 and 53 percent with medicinal and surgical interventions, respectively. Each approach has advantages and disadvantages. Manual therapy showed a decrease in pain for 84 percent of study participants, and a 93 percent improvement in sexual function.
Evidence on how effective medication is for relieving pain associated with endometriosis is limited.
The advantages of surgery are demonstrated efficacy for pain control, it is more effective for infertility than medicinal intervention, it provides a definitive diagnosis, and surgery can often be performed as a minimally invasive (laparoscopic) procedure to reduce morbidity and minimize the risk of post-operative adhesions. Efforts to develop effective strategies to reduce or prevent adhesions have been undertaken, but their formation remain a frequent side effect of abdominal surgery.
The advantages of physical therapy techniques are decreased cost, absence of major side-effects, it does not interfere with fertility, and near-universal increase of sexual function. Disadvantages are that there are no large or long-term studies of its use for treating pain or infertility related to endometriosis.
Treatment of infertility
Surgery is more effective than medicinal intervention for addressing infertility associated with endometriosis. Surgery attempts to remove endometrial tissue and preserve the ovaries without damaging normal tissue. In-vitro fertilization (IVF) procedures are effective in improving fertility in many women with endometriosis.
Prognosis
Proper counseling of women with endometriosis requires attention to several aspects of the disorder. Of primary importance is the initial operative staging of the disease to obtain adequate information on which to base future decisions about therapy. The woman's symptoms and desire for childbearing dictate appropriate therapy. Not all therapy works for all women. Some women have recurrences after surgery or pseudo-menopause. In most cases, treatment will give women significant relief from pelvic pain and assist them in achieving pregnancy.
The underlying process that causes endometriosis may not cease after a surgical or medical intervention. Studies have shown that endometriosis recurs at a rate of 20 to 40 percent within five years following conservative surgery, unless hysterectomy is performed or menopause reached. Monitoring of women consists of periodic clinical examinations and sonography.
Vaginal childbirth decreases recurrence of endometriosis. In contrast, endometriosis recurrence rates have been shown to be higher in women who have not given birth vaginally, such as in cesarean section.
Complications
Complications of endometriosis include internal scarring, adhesions, pelvic cysts, chocolate cyst of ovaries, ruptured cysts, and bowel and ureteral obstruction resulting from pelvic adhesions. Endometriosis-associated infertility can be related to scar formation and anatomical distortions due to the endometriosis.
Ovarian endometriosis may complicate pregnancy by decidualization, abscess and/or rupture.
Thoracic endometriosis is associated with recurrent pneumothoraces at times of a menstrual period, termed catamenial pneumothorax.
Epidemiology
Endometriosis can affect any female, from premenarche to postmenopause, regardless of race or ethnicity or whether or not they have had children. It is primarily a disease of the reproductive years. The number of women affected is between 6–10%. It is more common in women with infertility and chronic pelvic pain (35–50%).
Incidences of endometriosis have occurred in postmenopausal women, and in less common cases, girls may have endometriosis symptoms before they even reach menarche.
History
Endometriosis was first discovered microscopically by Karl von Rokitansky in 1860, although it was documented in medical texts more than 4,000 years ago. The Hippocratic Corpus outlines symptoms similar to endometriosis, including uterine ulcers, adhesions, and infertility. Historically, women with these symptoms were treated with leeches, straitjackets, bloodletting, chemical douches, genital mutilation, pregnancy (as a form of treatment), hanging upside down, surgical intervention, and even killing due to suspicion of demonic possession. Hippocratic doctors recognized and treated chronic pelvic pain as a true organic disorder 2,500 years ago, but during the Middle Ages, there was a shift into believing that women with pelvic pain were mad, immoral, imagining the pain, or simply misbehaving. The symptoms of inexplicable chronic pelvic pain were often attributed to imagined madness, female weakness, promiscuity, or hysteria. The historical diagnosis of hysteria, which was thought to be a psychological disease, may have indeed been endometriosis. The idea that chronic pelvic pain was related to mental illness influenced modern attitudes regarding women with endometriosis, leading to delays in correct diagnosis and indifference to the patients' true pain during the 20th century.
Hippocratic doctors believed that delaying childbearing could trigger diseases of the uterus, which caused endometriosis-like symptoms. Women with dysmenorrhea were encouraged to marry and have children at a young age. The fact that Hippocratics were recommending changes in marriage practices due to an endometriosis-like illness implies that this disease was likely common, with rates higher than the 5-15% prevalence that is often cited today. If indeed this disorder was so common historically, this may point away from modern theories that suggest links between endometriosis and dioxins, PCBs, and chemicals.
Society and culture
As recently as 1995, reports found that over 50% of women with chronic pelvic pain had no organic cause, with women still often being considered mentally unstable. Self-help groups say practitioners delay making the diagnosis, often because they don't consider it a possibility. In the US, as of 2007, about 27% of women with endometriosis had had the symptoms for at least six years before it is diagnosed.
The economic effects associated with endometriosis are substantial and are similar to that of other chronic diseases such as Crohn's disease, diabetes, or rheumatoid arthritis. This economic burden is attributed mostly to the inability to consistently work and predicted by decreased quality of life.
