Latin tunica mucosa uteri Dorlands/Elsevier Endometrium FMA 17742 | MeSH A05.360.319.679.490 TA A09.1.03.027 | |
 | ||
The endometrium is the inner epithelial layer, along with its mucous membrane, of the mammalian uterus. It has a basal layer and a functional layer; the functional layer thickens and then is sloughed during the menstrual cycle or estrous cycle. During pregnancy, the glands and blood vessels in the endometrium further increase in size and number. Vascular spaces fuse and become interconnected, forming the placenta, which supplies oxygen and nutrition to the embryo and fetus. The presence of commensal bacteria in the uterus and endometrium has been identified.
Contents
Structure
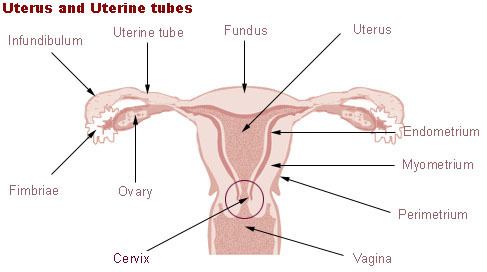
The endometrium consists of a single layer of columnar epithelium plus the stroma on which it rests. The stroma is a layer of connective tissue that varies in thickness according to hormonal influences. Simple tubular uterine glands reach from the endometrial surface through to the base of the stroma, which also carries a rich blood supply of spiral arteries. In a woman of reproductive age, two layers of endometrium can be distinguished. These two layers occur only in endometrium lining the cavity of the uterus, not in the lining of the uterine (Fallopian) tubes:
In the absence of progesterone, the arteries supplying blood to the functional layer constrict, so that cells in that layer become ischaemic and die, leading to menstruation.
It is possible to identify the phase of the menstrual cycle by reference to either the ovarian cycle or the uterine cycle by observing histological differences at each phase—for example in the ovarian cycle:
The first studies of flora colonizing the human endometrium were published in 2015, were on special populations, and were too small from which to generalize. In one study of 58 women undergoing hysterectomy, investigators looked for 12 species of bacteria; Lactobacillus and Prevotella were the most commonly detected species and overall density was much lower than vaginal colonization. In another study of 22 infertile women undergoing fertility treatments, Lactobacillus and Flavobacterium were most prevalent, and characteristics of the flora were roughly similar in women who became pregnant and those who didn't.
Function
The endometrium is the innermost glandular layer and functions as a lining for the uterus, preventing adhesions between the opposed walls of the myometrium, thereby maintaining the patency of the uterine cavity. During the menstrual cycle or estrous cycle, the endometrium grows to a thick, blood vessel-rich, glandular tissue layer. This represents an optimal environment for the implantation of a blastocyst upon its arrival in the uterus. The endometrium is central, echogenic (detectable using ultrasound scanners), and has an average thickness of 6.7 mm.
During pregnancy, the glands and blood vessels in the endometrium further increase in size and number. Vascular spaces fuse and become interconnected, forming the placenta, which supplies oxygen and nutrition to the embryo and fetus.
Cycle
The endometrial lining undergoes cyclic regeneration. Humans and the other great apes display the menstrual cycle, whereas most other mammals are subject to an estrous cycle. In both cases, the endometrium initially proliferates under the influence of estrogen. However, once ovulation occurs, in addition to estrogen, the ovary will also start to produce progesterone. This changes the proliferative pattern of the endometrium to a secretory lining. Eventually, the secretory lining provides a hospitable environment for one or more blastocysts.
Upon fertilization, the egg may implant into the uterine wall and provide feedback to the body with human chorionic gonadotropin (HCG). HCG provides continued feedback throughout pregnancy by maintaining the corpus luteum, which will continue its role of releasing progesterone and estrogen. The endometrial lining is either reabsorbed (estrous cycle) or shed (menstrual cycle). In the latter case, the process of shedding involves the breaking down of the lining, the tearing of small connective blood vessels, and the loss of the tissue and blood that had constituted it through the vagina. The entire process occurs over a period of several days. Menstruation may be accompanied by a series of uterine contractions; these help expel the menstrual endometrium.
In case of implantation, however, the endometrial lining is neither absorbed nor shed. Instead, it remains as decidua. The decidua becomes part of the placenta; it provides support and protection for the gestation.
If there is inadequate stimulation of the lining, due to lack of hormones, the endometrium remains thin and inactive. In humans, this will result in amenorrhea, or the absence of a menstrual period. After menopause, the lining is often described as being atrophic. In contrast, endometrium that is chronically exposed to estrogens, but not to progesterone, may become hyperplastic. Long-term use of oral contraceptives with highly potent progestins can also induce endometrial atrophy.
In humans, the cycle of building and shedding the endometrial lining lasts an average of 28 days. The endometrium develops at different rates in different mammals. Various factors including the seasons, climate, and stress can affect its development. The endometrium itself produces certain hormones at different stages of the cycle and this affects other parts of the reproductive system.
Clinical significance
Chorionic tissue can result in marked endometrial changes, known as an Arias-Stella reaction, that have an appearance similar to cancer. Historically, this change was diagnosed as endometrial cancer and it is important only in so far as it should not be misdiagnosed as cancer.
Thin endometrium may be defined as an endometrial thickness of less than 8 mm. It usually occurs after menopause. Treatments that can improve endometrial thickness include Vitamin E, L-arginine and sildenafil citrate.
Gene expression profiling using cDNA microarray can be used for the diagnosis of endometrial disorders. The European Menopause and Andropause Society (EMAS) released Guidelines with detailed information to assess the endometrium.
Embryo transfer
An endometrial thickness (EMT) of less than 7 mm decreases the pregnancy rate in in vitro fertilization by an odds ratio of approximately 0.4 compared to an EMT of over 7 mm. However, such low thickness rarely occurs, and any routine use of this parameter is regarded as not justified.
Observation of the endometrium by transvaginal ultrasonography is used when administering fertility medication, such as in in vitro fertilization. At the time of embryo transfer, it is favorable to have an endometrium of a thickness of between 7 and 14 mm with a triple-line configuration, which means that the endometrium contains a hyperechoic (usually displayed as light) line in the middle surrounded by two more hypoechoic (darker) lines. A triple-line endometrium reflects the separation of the stratum basalis and functionalis layers, and is also observed in the periovulatory period secondary to rising estradiol levels, and disappears after ovulation.
