 | ||
Fertility is the natural capability to produce offspring. As a measure, fertility rate is the number of offspring born per mating pair, individual or population. Fertility differs from fecundity, which is defined as the potential for reproduction (influenced by gamete production, fertilization and carrying a pregnancy to term). A lack of fertility is infertility while a lack of fecundity would be called sterility.
Contents
- Demography
- Period measures
- Cohort measures
- Social and economic determinants of fertility
- Bongaarts model of components of fertility
- Fertility biology
- Menstrual cycle
- Female fertility
- Male fertility
- France
- United States
- Post WWII
- Sexual revolution
- Infertility
- Journals
- References
Human fertility depends on factors of nutrition, sexual behavior, consanguinity, culture, instinct, endocrinology, timing, economics, way of life, and emotions.
Demography
In demographic contexts, fertility refers to the actual production of offspring, rather than the physical capability to produce which is termed fecundity. While fertility can be measured, fecundity cannot be. Demographers measure the fertility rate in a variety of ways, which can be broadly broken into "period" measures and "cohort" measures. "Period" measures refer to a cross-section of the population in one year. "Cohort" data on the other hand, follows the same people over a period of decades. Both period and cohort measures are widely used.
Period measures
Cohort measures
Social and economic determinants of fertility
A parent's number of children strongly correlates with the number of children that each person in the next generation will eventually have. Factors generally associated with increased fertility include religiosity, intention to have children, and maternal support. Factors generally associated with decreased fertility include wealth, education, female labor participation, urban residence, intelligence, increased female age and (to a lesser degree) increased male age.
The "Three-step Analysis" of the fertility process was introduced by Kingsley Davis and Judith Blake in 1956 and makes use of three proximate determinants: The economic analysis of fertility is part of household economics, a field that has grown out of the New Home Economics. Influential economic analyses of fertility include Becker (1960), Mincer (1963), and Easterlin (1969). The latter developed the Easterlin hypothesis to account for the Baby Boom.
Bongaarts' model of components of fertility
Bongaarts proposed a model where the total fertility rate of a population can be calculated from four proximate determinants and the total fecundity (TF). The index of marriage (Cm), the index of contraception (Cc), the index of induced abortion (Ca) and the index of postpartum infecundability (Ci). These indices range from 0 to 1. The higher the index, the higher it will make the TFR, for example a population where there are no induced abortions would have a Ca of 1, but a country where everybody used infallible contraception would have a Cc of 0.
TFR = TF × Cm × Ci × Ca × Cc
These four indices can also be used to calculate the total marital fertility (TMFR) and the total natural fertility (TN.
TFR = TMFR × Cm
TMFR = TN × Cc × Ca
TN = TF × Ci
Fertility biology
Women have hormonal cycles which determine when they can achieve pregnancy. The cycle is approximately twenty-eight days long, with a fertile period of five days per cycle, but can deviate greatly from this norm. Men are fertile continuously, but their sperm quality is affected by their health, frequency of ejaculation, and environmental factors.
Fertility declines with age in both sexes. In women the decline is more rapid, with complete infertility normally occurring around the age of 50.
Menstrual cycle
A woman's menstrual cycle begins, as it has been arbitrarily assigned, with menses. Next is the follicular phase where estrogen levels build as an ovum matures (due to the follicular stimulating hormone, or FSH) within the ovary. When estrogen levels peak, it spurs a surge of luteinizing hormone (LH) which finishes the ovum and enables it to break through the ovary wall. This is ovulation. During the luteal phase, which follows ovulation LH and FSH cause the post-ovulation ovary to develop into the corpus luteum which produces progesterone. The production of progesterone inhibits the LH and FSH hormones which (in a cycle without pregnancy) causes the corpus luteum to atrophy, and menses to begin the cycle again.
Peak fertility occurs during just a few days of the cycle: usually two days before and two days after the ovulation date. This fertile window varies from woman to woman, just as the ovulation date often varies from cycle to cycle for the same woman. The ovule is usually capable of being fertilized for up to 48 hours after it is released from the ovary. Sperm survive inside the uterus between 48 and 72 hours on average, with the maximum being 120 hours (5 days).
These periods and intervals are important factors for couples using the rhythm method of contraception.
Female fertility
The average age of menarche in the United States is about 12.5 years. In postmenarchal girls, about 80% of the cycles are anovulatory in the first year after menarche, 50% in the third and 10% in the sixth year.
Women's fertility peaks in the early 20s, and drops around age 35. Menopause occurs during a women's midlife ( between ages 48 and 55) During menopause, hormonal production by the ovaries is reduced, eventually causing a permanent cessation of the primary function of the ovaries, particularly the creation of the uterine lining (period). This is considered the end of the fertile phase of a woman's life.
According to a computer simulation run by Henri Leridon, PhD, an epidemiologist with the French Institute of Health and Medical Research, of women trying to get pregnant, without using fertility drugs or in vitro fertilization.
Studies of actual couples trying to conceive have come up with higher results: one 2004 study of 770 European women found that 82% of 35- to 39-year-old women conceived within a year, while another in 2013 of 2,820 Danish women saw 78% of 35- to 40-year-olds conceive within a year.
The use of fertility drugs and/or invitro fertilization can increase the chances of becoming pregnant at a later age. Successful pregnancies facilitated by fertility treatment have been documented in women as old as 67. Studies since 2004 now show that mammals may continue to produce new eggs throughout their lives, rather than being born with a finite number as previously thought. Researchers at the Massachusetts General Hospital in Boston, US, say that if eggs are newly created each month in humans as well, all current theories about the aging of the female reproductive system will have to be overhauled, although at this time this is simply conjecture.
According to the March of Dimes, "about 9 percent of recognized pregnancies for women aged 20 to 24 ended in miscarriage. The risk rose to about 20 percent at age 35 to 39, and more than 50 percent by age 42". Birth defects, especially those involving chromosome number and arrangement, also increase with the age of the mother. According to the March of Dimes, "At age 25, a woman has about a 1-in-1,250 chance of having a baby with Down syndrome; at age 30, a 1-in-1,000 chance; at age 35, a 1-in-400 chance; at age 40, a 1-in-100 chance; and at 45, a 1-in-30 chance."
Male fertility
Some research suggest that increased male age is associated with a decline in semen volume, sperm motility, and sperm morphology. In studies that controlled for female age, comparisons between men under 30 and men over 50 found relative decreases in pregnancy rates between 23% and 38%. It is suggested that sperm count declines with age, with men aged 50–80 years producing sperm at an average rate of 75% compared with men aged 20–50 years and that larger differences are seen in how many of the seminiferous tubules in the testes contain mature sperm:
Decline in male fertility is influenced by many factors, including lifestyle, environment and psychological factors. It has been proposed that foreplay might have a role increasing fertility rates and sperm quality in men, but more research needs to be conducted.
Some research also suggests increased risks for health problems for children of older fathers, but no clear association has been proven. A large scale in Israel study suggested that the children of men 40 or older were 5.75 times more likely than children of men under 30 to have an autism spectrum disorder, controlling for year of birth, socioeconomic status, and maternal age. Increased paternal age is suggested by some to directly correlate to schizophrenia but it is not proven.
Australian researchers have found evidence to suggest overweight obesity may cause subtle damage to sperm and prevent a healthy pregnancy. They say fertilization was 40% less likely to succeed when the father was overweight.
The American Fertility Society recommends an age limit for sperm donors of 50 years or less, and many fertility clinics in the United Kingdom will not accept donations from men over 40 or 45 years of age.
France
The French pronatalist movement from 1919–1945 failed to convince French couples of having a patriotic duty to help increase their country's birthrate. Even the government was reluctant in its support to the movement. It was only between 1938 and 1939 that the French government became directly and permanently involved in the pronatalist effort. Although the birthrate started to surge in late 1941, the trend was not sustained. Falling birthrate once again became a major concern among demographers and government officials beginning in the 1970s.
United States
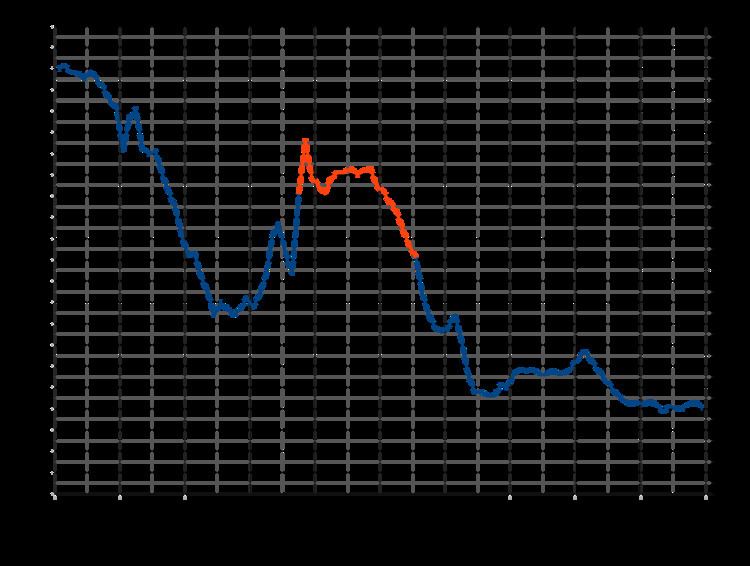
From 1800 to 1940, fertility fell in the US. There was a marked decline in fertility in the early 1900s, associated with improved contraceptives, greater access to contraceptives and sexuality information and the "first" sexual revolution.
Post-WWII
After 1940 fertility suddenly started going up again, reaching a new peak in 1957. After 1960, fertility started declining rapidly. In the Baby Boom years (1946–1964), women married earlier and had their babies sooner; the number of children born to mothers after age 35 did not increase.
Sexual revolution
After 1960, new methods of contraception became available, ideal family size fell, from 3 to 2 children. Couples postponed marriage and first births, and they sharply reduced the number of third and fourth births.
Infertility
Infertility primarily refers to the biological inability of a person to contribute to conception. Infertility may also refer to the state of a woman who is unable to carry a pregnancy to full term. There are many biological causes of infertility, including some that medical intervention can treat.
