 | ||
Obesity is defined as an abnormal accumulation of body fat, usually 20% or more over an individual's ideal body weight. This is often described as a body mass index (BMI) over 30. However, BMI does not account for whether the excess weight is fat or muscle, and is not a measure of body composition. For most people, however, BMI is an indication used worldwide to estimate nutritional status. Obesity is usually the result of consuming more calories than the body needs and not expanding that energy by doing exercise. There are genetic causes and hormonal disorders that causes people to gain significant amounts of weight but this is rare. People in the obese category are much more likely to suffer from fertility problems than people of normal healthy weight.
Contents
A report carried out by the Nurses Health Study demonstrated an increased risk of anovulation in women with an increasing BMI value. Its major effects include a reduction in ovulation rate, a decline in oocyte quality, menstrual irregularities, a decreased pregnancy rate and a rise in miscarriages. Obesity can have particularly damaging effects in young women as they begin menstruating earlier than normal girls, essentially enhancing the defects associated with obesity and fertility. Obesity also has an impact on fertility in men.
Women
The hormones involved in the reproductive system are negatively affected with an increase of weight. In humans, via white adipocytes (fat cells), production of the hormone leptin (an adipokine) acts on the hypothalamus where reproductive hormone Gonadotrophin-releasing hormone (GnRH) is produced. Leptin is also a product of the obese gene. Leptins interaction with the hypothalamus decreases appetite, therefore a mutation in the obese gene would result in an increased appetite, leading to inevitable obesity. Leptin has been found to be linked to the HPG axis as it can induce the release of GnRH by the hypothalamus and subsequently follicle stimulating hormone (FSH) and leutinising hormone (LH) by the anterior pituitary. Pre-pubertal individuals that lack leptin fail to reach the pubertal stage. If given leptin administratively, the mutation would be reversed and puberty resumed. Leptin is further expressed in mature follicles produced by the ovary, suggesting it plays a role in oocyte maturation, hence embryo development.
Increasing body weight is also thought to be linked to the development of polycystic ovary syndrome (PCOS). There are specific aspects associated with PCOS allowing an indication of diagnosis of the syndrome including hyperandrogenism (hirsutism), irregular periods, anovulation and subfertility. Obesity in PCOS sufferers amplifies hormonal and metabolic decline, therefore damaging fertility and oocyte quality in women. PCOS can also have an effect if conception is successful through assisted reproductive technology (ART) in obese patients, leading to an increase in miscarriage rates.
Polycystic ovarian syndrome
PCOS is a very common endocrine disorder among women who are reproductively active. Hyperandrogenism is a medical condition where there are excessive levels of androgens in the body. It is associated with PCOS. Studies have shown that hyperandrogenism could be caused by a reaction between ovarian theca cells and reactive oxygen species. Obesity interferes with the HPA axis and stops follicular maturation. Hyperandrogenism has a disturbing effect on this process and could cause anovulatory cycles. Currently, therapy is aimed at patients that need to improve their resistance to insulin so that hyperinsulinemia is reduced and ovulatory features in women are improved. According to recent studies, insulin-sensitiser drugs are the main type of therapy for women with irregular cycles that want to improve their fertility, although weight loss is normally the first step in overweight patients with PCOS.
Men
Obese men have lower circulating testosterone which affects sperm production known as spermatogenesis. This affects the quantity and quality of a mans sperm. Obese men have increased risk of oligozoospemia, having fewer than 15 million sperm per millilitre of semen, and far fewer motile sperm than a man of healthy weight. Sperm with high amounts of damaged DNA are significantly more common in obese men than in normal weight men. Ejaculate volume is also affected. Altered male hormones will can also give erectile dysfunction which is the major cause of infertility in obese men.
Female
Preventing or treating obesity in women has a positive effect on fertility rates. As simple as modifying lifestyle choices in order to lose weight could lead to a recovery in fertility decline. Taken into consideration firstly must be the weight of the individual before investigating further into complications surrounding fertility. Initially, treatment should proceed for obesity, then if complications still arise with infertility then progression onto ART is required. There are many other ways of reducing body fat including modifying diet or administrating diet pills, increasing energy expenditure, or surgically removing abdominal fat/surgical fitting of a gastric band in order to subside excess abdominal weight. Restoration of fertility should follow these modifications. A weight-loss study was carried out of 13 individuals over a 6-month period. 12 of the 13 previously infertile subjects restored ovulation whilst 11 subjects were able to conceive after the programme had ended. This study demonstrates weight loss to be the primary source of treatment for obesity and fertility problems before ART. A further study enhances this idea with 80% of females having regular menstrual cycles and conception rate was 29% after modifications.
Male
Impacts of obesity on male fertility can be reversed, either with testosterone therapy, or weight loss. Testosterone therapy is likely to improve hormone imbalances and treat erectile dysfunction. Weight loss can be achieved through lifestyle changes such as a reduced calorie diet, regular exercise and quitting smoking. Trained healthcare professionals and weight loss groups may also be beneficial. People struggling to keep to these lifestyle changes may seek other methods such as medication known as orlistat or weight loss surgery.
Cattle
It is common practise for body condition scoring to be used in domesticated animals to assess the fatness of an animal and is often used by vets and livestock handlers to determine whether the animal need more or less energy. Both a low and a high score can negatively impact an animal’s fertility.
Cattle that are over-conditioned are also more insulin resistant compared to their leaner counterparts. As demonstrated in mice, insulin resistance is a factor in poor fertility as it has an effect on oocyte development. This in turn means that less oocytes are suitable for fertilisation and fertility is impaired.
Another reason for decrease in fertility is to do with leptin. Leptin is a hormone which production is increased in obese animals. In cows, leptin can inhibit thecal cells from producing adrostenediol and progesterone. Androstenediol is important in fertility as it is the precursor to oestrogen. Without oestrogen production, the balance of hormones is affected and there is no LH surge with is required for ovulation.
Domestic Fowl
Domestic fowl has previously been researched on and it was found that by over feeding but not force feeding the male birds, there was no impact on fertility. However, more recently a study has shown that obesity induced by force feeding can have an impact on the number of spermatozoa and their motility in the male birds. It was also found that in two of the three birds, there was an decrease in testosterone and an increase in LH which suggests the pathway of why there might be reduced spermatozoa.
Epidemiology
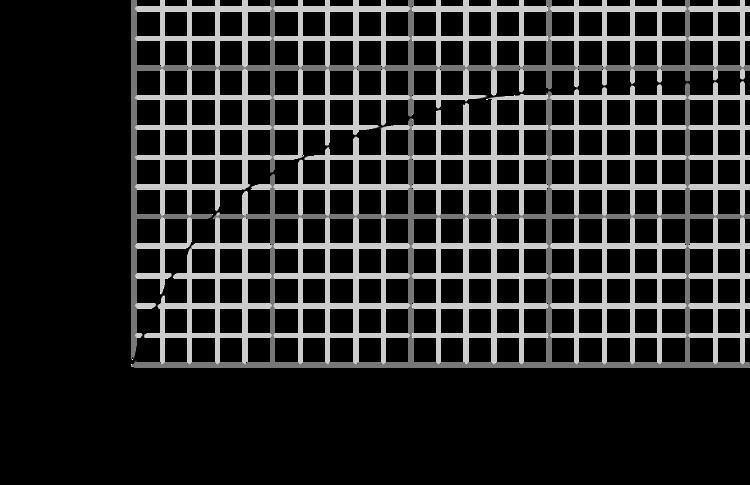
Many women who have PCOS are also obese and it is estimated that the prevalence of obesity in women with PCOS is 35 - 63%. It has also been shown that there is a relative risk of anovulatory infertility in amongst the obese population is 2.7%. For those who are obese and are ovulatory, for each unit increase in BMI over a BMI of 32 kg/m² at the age of 18, there is a reduction of spontaneous conception rate by 5%.
