System Circulatory system FMA 50723 | Latin vena | |
 | ||
TA A12.0.00.030A12.3.00.001 | ||
Veins are blood vessels that carry blood toward the heart. Most veins carry deoxygenated blood from the tissues back to the heart; exceptions are the pulmonary and umbilical veins, both of which carry oxygenated blood to the heart. In contrast to veins, arteries carry blood away from the heart.
Contents
- Structure
- Venous system
- Microanatomy
- Function
- Venous insufficiency
- Deep vein thrombosis
- Portal hypertension
- Other
- Imaging
- Veins of clinical significance
- Phlebology
- History
- References
Veins are less muscular than arteries and are often closer to the skin. There are valves in most veins to prevent backflow.
Structure
Veins are present throughout the body as tubes that carry blood back to the heart. Veins are classified in a number of ways, including superficial vs. deep, pulmonary vs. systemic, and large vs. small.
Most veins are equipped with valves to prevent blood flowing in the reverse direction.
Veins are translucent, so the color a vein appears from an organism's exterior is determined in large part by the color of venous blood, which is usually dark red as a result of its low oxygen content. Veins appear blue because the subcutaneous fat absorbs low-frequency light, permitting only the highly energetic blue wavelengths to penetrate through to the dark vein and reflect back to the viewer. The colour of a vein can be affected by the characteristics of a person's skin, how much oxygen is being carried in the blood, and how big and deep the vessels are. When a vein is drained of blood and removed from an organism, it appears grey-white.
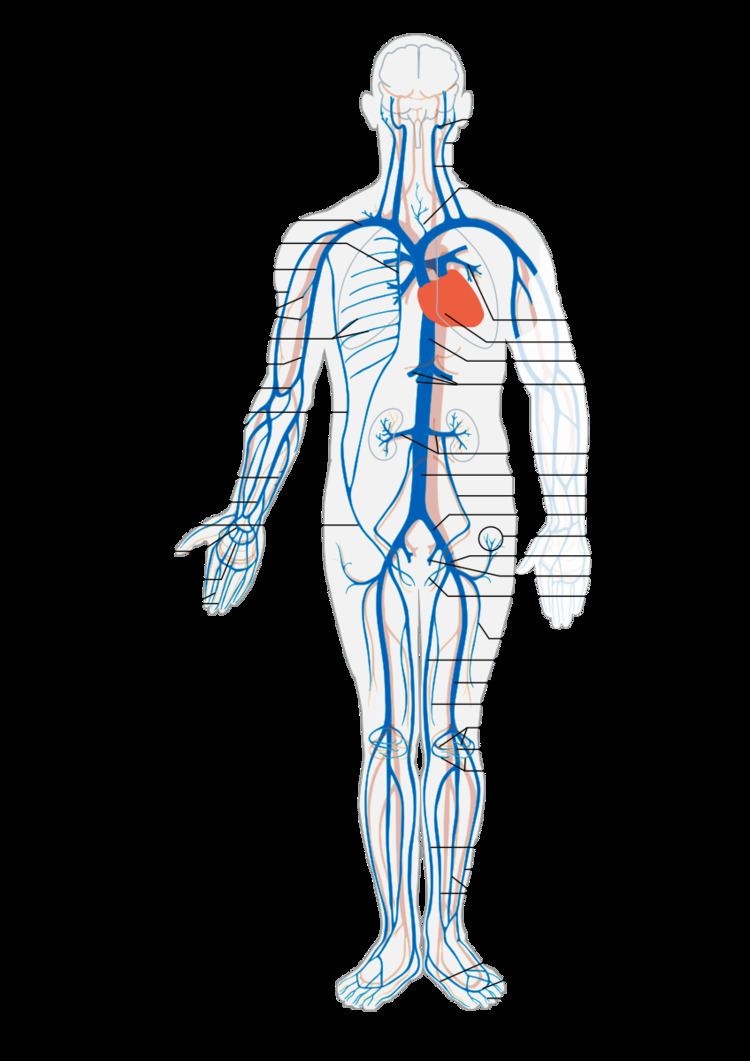
Venous system
The largest veins in the human body are the venae cavae. These are two large veins which enter the right atrium of the heart from above and below. The superior vena cava carries blood from the arms and head to the right atrium of the heart, while the inferior vena cava carries blood from the legs and abdomen to the heart. The inferior vena cava is retroperitoneal and runs to the right and roughly parallel to the abdominal aorta along the spine. Large veins feed into these two veins, and smaller veins into these. Together this forms the venous system.
Whilst the main veins hold a relatively constant position, the position of veins person to person can display quite a lot of variation.
The pulmonary veins carry relatively oxygenated blood from the lungs to the heart. The superior and inferior venae cavae carry relatively deoxygenated blood from the upper and lower systemic circulations, respectively.
The portal venous system is a series of veins or venules that directly connect two capillary beds. Examples of such systems include the hepatic portal vein and hypophyseal portal system.
The peripheral veins carry blood from the limbs and hands and feet.
Microanatomy
Microscopically, veins have a thick outer layer made of connective tissue, called the tunica externa or tunica adventitia. There is a middle layer of bands of smooth muscle called tunica media, which are, in general, much thinner than those of arteries, as veins do not function primarily in a contractile manner and are not subject to the high pressures of systole, as arteries are. The interior is lined with endothelial cells called tunica intima. The precise location of veins varies much more from person to person than that of arteries.
Function
Veins serve to return blood from organs to the heart. Veins are also called "capacitance vessels" because most of the blood volume (60%) is contained within veins. In systemic circulation oxygenated blood is pumped by the left ventricle through the arteries to the muscles and organs of the body, where its nutrients and gases are exchanged at capillaries. After taking up cellular waste and carbon dioxide in capillaries, blood is channeled through vessels that converge with one another to form venules, which continue to converge and form the larger veins. The de-oxygenated blood is taken by veins to the right atrium of the heart, which transfers the blood to the right ventricle, where it is then pumped through the pulmonary arteries to the lungs. In pulmonary circulation the pulmonary veins return oxygenated blood from the lungs to the left atrium, which empties into the left ventricle, completing the cycle of blood circulation.
The return of blood to the heart is assisted by the action of the muscle pump, and by the thoracic pump action of breathing during respiration. Standing or sitting for a prolonged period of time can cause low venous return from venous pooling (vascular) shock. Fainting can occur but usually baroreceptors within the aortic sinuses initiate a baroreflex such angiotensin II and norepinephrine stimulate vasoconstriction and heart rate increases to return blood flow. Neurogenic and hypovolaemic shock can also cause fainting. In these cases, the smooth muscles surrounding the veins become slack and the veins fill with the majority of the blood in the body, keeping blood away from the brain and causing unconsciousness. Jet pilots wear pressurized suits to help maintain their venous return and blood pressure.
The arteries are perceived as carrying oxygenated blood to the tissues, while veins carry deoxygenated blood back to the heart. This is true of the systemic circulation, by far the larger of the two circuits of blood in the body, which transports oxygen from the heart to the tissues of the body. However, in pulmonary circulation, the arteries carry deoxygenated blood from the heart to the lungs, and veins return blood from the lungs to the heart. The difference between veins and arteries is their direction of flow (out of the heart by arteries, returning to the heart for veins), not their oxygen content. In addition, deoxygenated blood that is carried from the tissues back to the heart for reoxygenation in systemic circulation still carries some oxygen, though it is considerably less than that carried by the systemic arteries or pulmonary veins.
Although most veins take blood back to the heart, there is an exception. Portal veins carry blood between capillary beds. For example, the hepatic portal vein takes blood from the capillary beds in the digestive tract and transports it to the capillary beds in the liver. The blood is then drained in the gastrointestinal tract and spleen, where it is taken up by the hepatic veins, and blood is taken back into the heart. Since this is an important function in mammals, damage to the hepatic portal vein can be dangerous. Blood clotting in the hepatic portal vein can cause portal hypertension, which results in a decrease of blood fluid to the liver.
Venous insufficiency
Venous insufficiency is the most common disorder of the venous system, and is usually manifested as spider veins or varicose veins. Several varieties of treatments are used, depending on the patient's particular type and pattern of veins and on the physician's preferences. Treatment can include Endovenous Thermal Ablation using radiofrequency or laser energy, vein stripping, ambulatory phlebectomy, foam sclerotherapy, lasers, or compression.
Postphlebitic syndrome is venous insufficiency that develops following deep vein thrombosis.
Deep vein thrombosis
Deep vein thrombosis is a condition in which a blood clot forms in a deep vein. This is usually the veins of the legs, although it can also occur in the veins of the arms. Immobility, active cancer, obesity, traumatic damage and congenital disorders that make clots more likely are all risk factors for deep vein thrombosis. It can cause the affected limb to swell, and cause pain and an overlying skin rash. In the worst case, a deep vein thrombosis can extend, or a part of a clot can break off and land in the lungs, called pulmonary embolism.
The decision to treat deep vein thrombosis depends on its size, a person's symptoms, and their risk factors. It generally involves anticoagulation to try and reduce and prevent the size of the clot.
Portal hypertension
The portal veins are found within the abdomen and carry blood through to the liver. Portal hypertension is associated with cirrhosis or disease of the liver, or other conditions such as an obstructing clot (Budd Chiari syndrome) or compression from tumours or tuberculosis lesions. When the pressure increases in the portal veins, a collateral circulation develops, causing visible veins such as oesophageal varices.
Other
Thrombophlebitis is an inflammatory condition of the veins related to blood clots.
Imaging
Ultrasound, particularly duplex ultrasound, is a common way that veins can be seen.
Veins of clinical significance
The Batson Venous plexus, or simply Batson's Plexus, runs through the inner vertebral column connecting the thoracic and pelvic veins. These veins get their notoriety from the fact that they are valveless, which is believed to be the reason for metastasis of certain cancers.
The great saphenous vein is the most important superficial vein of the lower limb. First described by the Persian physician Avicenna, this vein derives its name from the word safina, meaning "hidden". This vein is "hidden" in its own fascial compartment in the thigh and exits the fascia only near the knee. Incompetence of this vein is an important cause of varicose veins of lower limbs.
The Thebesian veins within the myocardium of the heart are valveless veins that drain directly into the chambers of the heart. The coronary veins all empty into the coronary sinus which empties into the right atrium.
The dural venous sinuses within the dura mater surrounding the brain receive blood from the brain and also are a point of entry of cerebrospinal fluid from arachnoid villi absorption. Blood eventually enters the internal jugular vein.
Phlebology
Phlebology is the medical specialty devoted to the diagnosis and treatment of venous disorders. A medical specialist in phlebology is termed a phlebologist. A related image is called a phlebograph.
The American Medical Association added phlebology to their list of self-designated practice specialties in 2005. In 2007, the American Board of Phlebology (ABPh), now known as the American Board of Venous & Lymphatic Medicine (ABVLM), was established to improve the standards of phlebologists and the quality of their patient care by establishing a certification examination, as well as requiring maintenance of certification. Although not currently a Member Board of the American Board of Medical Specialties (ABMS); the American Board of Venous & Lymphatic Medicine certification exam is based on ABMS standards. The American College of Phlebology (ACP) is one of the largest medical societies in the world for physicians and allied health professionals working in the field of phlebology. The ACP has 2000 members. The ACP encourages education and training to improve the standards of medical practitioners and the quality of patient care. The American Venous Forum (AVF) is a medical society for physicians and allied health professionals dedicated to improving the care of patients with venous and lymphatic disease. The majority of its members manage the entire spectrum of venous and lymphatic diseases – from varicose veins, to congenital abnormalities to deep vein thrombosis to chronic venous diseases. Founded in 1987, the AVF encourages research, clinical innovation, hands-on education, data collection and patient outreach.
The ACP is part of the UIP (International Union of Phlebology). The equivalent body for countries in the Pacific is the Australasian College of Phlebology, active in Australia and New Zealand.
History
The valves in veins were described by Jacques Dubois, but their true function was later discovered by William Harvey.
