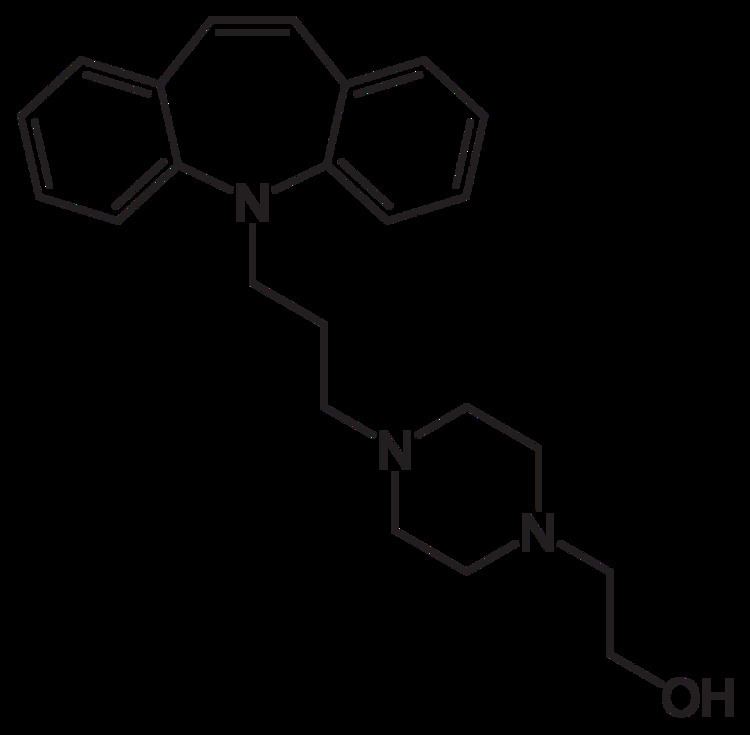
Trade names Insidon, Opipram ATC code N06AA05 (WHO) Molar mass 363.496 g/mol | Bioavailability 94% | |
 | ||
AHFS/Drugs.com International Drug Names Legal status In general: ℞ (Prescription only) | ||
Opipramol (Insidon, Pramolan, Ensidon, Oprimol) is an antidepressant and anxiolytic used in Germany and other European countries. Although it is a member of the tricyclic antidepressants, opipramol's primary mechanism of action is much different in comparison. Most TCAs act as reuptake inhibitors, but opipramol does not, and instead acts as a sigma receptor agonist, among other properties. It is an iminostilbene derivative, belonging to dibenzazepine group. Opipramol was developed by Schindler and Blattner in 1961.
Contents
- Medical vocabulary what does opipramol mean
- Medical uses
- Pregnancy and lactation
- Pharmacology
- Pharmacokinetics
- Adverse effects
- Overdosage
- Drug interactions
- Contraindications
- References
Medical vocabulary what does opipramol mean
Medical uses
Opipramol is typically used in the treatment of generalized anxiety disorder (GAD) and somatoform disorders. Its anxiolysis becomes prominent after only one to two weeks of chronic administration. Upon first commencing treatment, opipramol is rather sedating in nature due to its antihistamine properties, but this effect becomes less prominent with time.
Opipramol's sigma-1 agonistic effects likely impart potent antitussive effects, many other sigma-1 agonists (ex. codeine, hydrocodone, and dextromethorphan) are used for this purpose.
Pregnancy and lactation
Experimental animal studies did not indicate injurious effects of opipramol on the embryonic development or the fertility. Opipramol should be prescribed during pregnancy, particularly in the first trimester, only for compelling indication. Opipramol should not be used during lactation period, since the active ingredient passes into the milk in small quantities.
Pharmacology
Opipramol acts as a high affinity sigma receptor agonist, primarily at the σ1 subtype, but also at the σ2 subtype with somewhat lower affinity. It is this property which is responsible for its therapeutic benefits against anxiety and depression. Opipramol also acts as a low to moderate affinity antagonist for the D2, 5-HT2, H1, H2, and muscarinic acetylcholine receptors. H1 and H2 receptor antagonism account for its antihistamine effects, and muscarinic acetylcholine receptor antagonism is responsible for its anticholinergic properties. Sigma receptors are a set of proteins located in the endoplasmic reticulum. σ1 receptors play key role in potentiating intracellular calcium mobilization thereby acting as sensor or modulator of calcium signalling. Occupancy of σ1 receptors by agonists causes translocation of the receptor from endoplasmic reticulum to peripheral areas (membranes) where the σ1 receptors cause neurotransmitter release. The biphasic action initially makes prompt improvement of tension, anxiety and insomnia. Opipramol is a tranquilizer with a thymoleptic component. After sub-chronic treatment with opipramol σ2 receptors are significantly down-regulated- but not σ1 receptors.
Pharmacokinetics
Opipramol is rapidly and completely absorbed by the gastrointestinal tract. Its terminal plasma half life is 6–11 hours. After single oral administration of 50 mg, the peak plasma concentration of the drug is reached after 3.3 hours and amounts to 15.6 ng/ml. After single oral administration of 100 mg the maximum plasma concentration is reached after 3 hours and amounts to 33.2 ng/ml. The bioavailability of opipramol amounts to 94%. The plasma protein binding amounts to approximately 91% and the volume of distribution is approximately 10 L/kg. Opipramol is partially metabolized in liver as deshydroxy ethyl-opipramol. Metabolization occurs through CYP2D6-isoenzyme. 70% is eliminated renally and 10% unaltered. Remaining portion is eliminated through faeces.
Adverse effects
Opipramol is a well-tolerated drug and produces fewer side effects than SSRIs and SNRIs.
The frequently (≥1% to <10%) reported adverse reactions with opipramol especially at the beginning of the treatment includes fatigue, dry mouth, blocked nose, hypotension and orthostatic dysregulation.
The adverse reactions reported occasionally(≥0.1% to <1%) includes dizziness, stupor, micturition disturbances, accommodation disturbances, tremor, weight gain, thirst, allergic skin reactions (rash, uriticaria), abnormal ejaculation, erectile impotence, constipation, transient increase in liver enzyme activities, tachycardia and palpilations.
Rarely (≥0.01% to <0.1%) reported adverse reaction includes excitation, headache, parethesia especially in elderly patients, restlessness, sweating, sleep disturbances, oedema, galactorrhea, urine blockage, nausea and vomiting, collapse conditions, stimulation conducting disturbances, intensification of present heart insufficiency, blood profile changes particularly leukopenia, confusion, delirium, stomach complaints, taste disturbance and paralytic ileus especially with sudden discontinuation of a longer-term high-dose therapy.
Very rarely (<0.01%) adverse reaction includes seizures, motor disorder, (akathisia, dyskinesia), ataxia, polyneuropathy, glaucoma, anxiety, hairfall, agranulocytosis, severe liver dysfunction after long-term treatment, jaundice and chronic liver damage.
Overdosage
Symptoms of intoxications includes drowsiness, insomnia, stupor, agitation, coma, transient confusion, increased anxiety, ataxia, convulsions, oligouria, anuria, tachycardia or bradycardia, arrhythmia, AV block, hypotension, shock, respiratory depression, rarely, cardiac arrest.
As therapy of intoxication, specific antidote is not available, removal of the drug by vomiting or gastric lavage should be done. Continuous cardiovascular monitoring for at least 48 hours should be done. In case of respiratory failure due to overdose, intubation and artificial respiration should be done. During severe hypotension due to overdose, corresponding recumbent positioning, plasma expander, dopamine or dobutamine as drops-infusion should be initiated. In heart rhythm disturbances, individualized treatment should be done where appropriate pacemaker and compensation in low potassium levels and possible acidosis should be done. While in convulsions due to overdose, administration of intravenous diazepam or another anti-convulsant agent such as phenobarbital or paraldehyde should be done though intensification of existing respiratory insufficiency, hypotension or coma may happen.
Drug interactions
The therapy with Opipramol indicates an additional therapy with neuroleptics, hypnotics and tranquilizers (e.g. Barbiturates, Benzodiazepines). Therefore, it should be noted that some specific reactions, particularly CNS depressant effects could be intensified and an intensification of common side effects may occur. If necessary the dosage may be reduced. Co-administration with alcohol can cause stupor. MAO Inhibitors should be discontinued at least 14 days before the treatment with Opipramol. Concomitant use of Opipramol with β-blockers, antiarrhythmics (of class 1c), as well as drugs from tricyclic antidepressant group and preparations which influence the microsomal enzyme system, can lead to change in plasma concentration of these drugs. Co-administration of neuroleptics (example- haloperidol, risperidone) can increase the plasma concentration. Barbiturates and anticonvulsants can reduce the plasma concentration of Opipramol and thereby weaken the therapeutic effect.
