Entrez 3569 | Ensembl ENSG00000136244 | |
 | ||
External IDs OMIM: 147620 MGI: 96559 HomoloGene: 502 GeneCards: IL6 | ||
Interleukin 6 (IL-6) is an interleukin that acts as both a pro-inflammatory cytokine and an anti-inflammatory myokine. In humans, it is encoded by the IL6 gene.
Contents
- Function
- Role as myokine
- Receptor
- Interactions
- Role in disease
- Rheumatoid arthritis
- Cancer
- Enterovirus 71
- Epigenetic modifications
- Schizophrenia
- Depression and major depressive disorder
- Asthma
- References
Interleukin 6 is secreted by T cells and macrophages to stimulate immune response, e.g. during infection and after trauma, especially burns or other tissue damage leading to inflammation. IL-6 also plays a role in fighting infection, as IL-6 has been shown in mice to be required for resistance against bacterium Streptococcus pneumoniae.
In addition, osteoblasts secrete IL-6 to stimulate osteoclast formation. Smooth muscle cells in the tunica media of many blood vessels also produce IL-6 as a pro-inflammatory cytokine. IL-6's role as an anti-inflammatory cytokine is mediated through its inhibitory effects on TNF-alpha and IL-1, and activation of IL-1ra and IL-10.
Function
IL-6 is an important mediator of fever and of the acute phase response. It is capable of crossing the blood-brain barrier and initiating synthesis of PGE2 in the hypothalamus, thereby changing the body's temperature setpoint. In muscle and fatty tissue, IL-6 stimulates energy mobilization that leads to increased body temperature. IL-6 can be secreted by macrophages in response to specific microbial molecules, referred to as pathogen-associated molecular patterns (PAMPs). These PAMPs bind to an important group of detection molecules of the innate immune system, called pattern recognition receptors (PRRs), including Toll-like receptors (TLRs). These are present on the cell surface and intracellular compartments and induce intracellular signaling cascades that give rise to inflammatory cytokine production.
IL-6 is also essential for hybridoma growth and is found in many supplemental cloning media such as briclone. Inhibitors of IL-6 (including estrogen) are used to treat postmenopausal osteoporosis. IL-6 is also produced by adipocytes and is thought to be a reason why obese individuals have higher endogeneous levels of CRP. Intranasally administered IL-6 has been shown to improve sleep-associated consolidation of emotional memories.
IL-6 is responsible for stimulating acute phase protein synthesis, as well as the production of neutrophils in the bone marrow. It supports the growth of B cells and is antagonistic to regulatory T cells.
When psychologically stressed, the human body produces stress hormones like cortisol, which are able to trigger interleukin-6 release into the circulation. Interleukin-6's antagonistic position to T-Cells, seems to be at least partly mediated by the inhibiting effect of PGE2 on the signaling function of T-Cells. PGE2 gets released in response to an activation by IL-6, leading not only to a greater chance of catching a virus but increasing the chance that a disease develops some sort of severity before the immune system fully kicks in. It is mainly the T4-helper-cells that have an important signaling function, either communicating B-Cells to produce antibodies or informing killer T-Cells about certain antigens that need to be destroyed. Therefore IL-6 seems to play a major role in the process of acute or chronic stress (f.e. depression, anxiety) suppressing the immune system. High levels of IL-6 in cancer-patients or in children with encephalitis (as mentioned below) could therefore be explained by the high levels of psychological stress these diseases trigger in the patients minds.
Role as myokine
IL-6 is also considered a myokine, a cytokine produced from muscle, which is elevated in response to muscle contraction. It is significantly elevated with exercise, and precedes the appearance of other cytokines in the circulation. During exercise, it is thought to act in a hormone-like manner to mobilize extracellular substrates and/or augment substrate delivery.
IL-6 has extensive anti-inflammatory functions in its role as a myokine. IL-6 was the first myokine that was found to be secreted into the blood stream in response to muscle contractions. Aerobic exercise provokes a systemic cytokine response, including, for example, IL-6, IL-1 receptor antagonist (IL-1ra), and IL-10. IL-6 was serendipitously discovered as a myokine because of the observation that it increased in an exponential fashion proportional to the length of exercise and the amount of muscle mass engaged in the exercise. It has been consistently demonstrated that the plasma concentration of IL-6 increases during muscular exercise. This increase is followed by the appearance of IL-1ra and the anti-inflammatory cytokine IL-10. In general, the cytokine response to exercise and sepsis differs with regard to TNF-α. Thus, the cytokine response to exercise is not preceded by an increase in plasma-TNF-α. Following exercise, the basal plasma IL-6 concentration may increase up to 100-fold, but less dramatic increases are more frequent. The exercise-induced increase of plasma IL-6 occurs in an exponential manner and the peak IL-6 level is reached at the end of the exercise or shortly thereafter. It is the combination of mode, intensity, and duration of the exercise that determines the magnitude of the exercise-induced increase of plasma IL-6.
IL-6 had previously been classified as a proinflammatory cytokine. Therefore, it was first thought that the exercise-induced IL-6 response was related to muscle damage. However, it has become evident that eccentric exercise is not associated with a larger increase in plasma IL-6 than exercise involving concentric "nondamaging" muscle contractions. This finding clearly demonstrates that muscle damage is not required to provoke an increase in plasma IL-6 during exercise. As a matter of fact, eccentric exercise may result in a delayed peak and a much slower decrease of plasma IL-6 during recovery.
Recent work has shown that both upstream and downstream signalling pathways for IL-6 differ markedly between myocytes and macrophages. It appears that unlike IL-6 signalling in macrophages, which is dependent upon activation of the NFκB signalling pathway, intramuscular IL-6 expression is regulated by a network of signalling cascades, including the Ca2+/NFAT and glycogen/p38 MAPK pathways. Thus, when IL-6 is signalling in monocytes or macrophages, it creates a pro-inflammatory response, whereas IL-6 activation and signalling in muscle is totally independent of a preceding TNF-response or NFκB activation, and is anti-inflammatory.
IL-6, among an increasing number of other recently identified myokines, thus remains an important topic in myokine research. It appears in muscle tissue and in the circulation during exercise at levels up to one hundred times basal rates, as noted, and is seen as having a beneficial impact on health and bodily functioning when elevated in response to physical exercise. IL-6 was the first myokine that was found to be secreted into the blood stream in response to muscle contractions.
Receptor
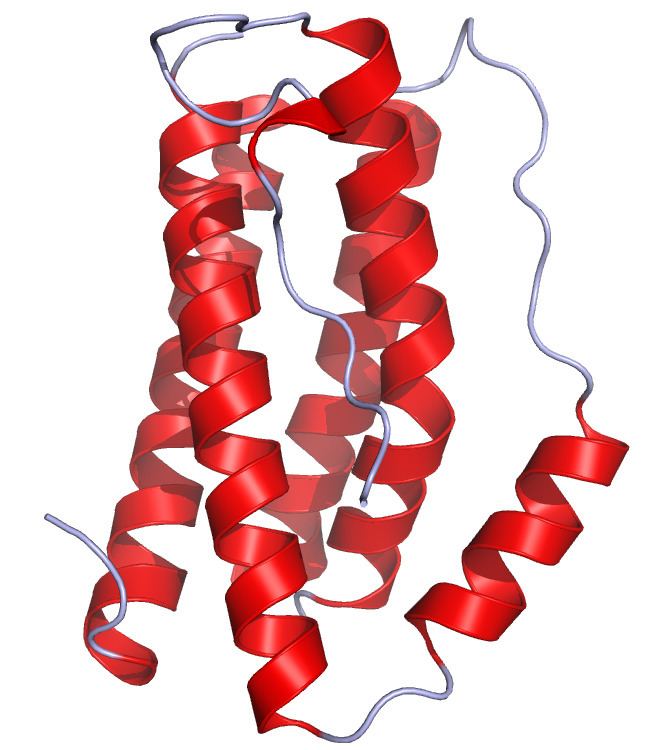
IL-6 signals through a cell-surface type I cytokine receptor complex consisting of the ligand-binding IL-6Rα chain (CD126), and the signal-transducing component gp130 (also called CD130). CD130 is the common signal transducer for several cytokines including leukemia inhibitory factor (LIF), ciliary neurotropic factor, oncostatin M, IL-11 and cardiotrophin-1, and is almost ubiquitously expressed in most tissues. In contrast, the expression of CD126 is restricted to certain tissues. As IL-6 interacts with its receptor, it triggers the gp130 and IL-6R proteins to form a complex, thus activating the receptor. These complexes bring together the intracellular regions of gp130 to initiate a signal transduction cascade through certain transcription factors, Janus kinases (JAKs) and Signal Transducers and Activators of Transcription (STATs).
IL-6 is probably the best-studied of the cytokines that use gp130, also known as IL-6 signal transducer (IL6ST), in their signalling complexes. Other cytokines that signal through receptors containing gp130 are Interleukin 11 (IL-11), Interleukin 27 (IL-27), ciliary neurotrophic factor (CNTF), cardiotrophin-1 (CT-1), cardiotrophin-like cytokine (CLC), leukemia inhibitory factor (LIF), oncostatin M (OSM), Kaposi's sarcoma-associated herpesvirus interleukin 6-like protein (KSHV-IL6). These cytokines are commonly referred to as the IL-6 like or gp130 utilising cytokines
In addition to the membrane-bound receptor, a soluble form of IL-6R (sIL-6R) has been purified from human serum and urine. Many neuronal cells are unresponsive to stimulation by IL-6 alone, but differentiation and survival of neuronal cells can be mediated through the action of sIL-6R. The sIL-6R/IL-6 complex can stimulate neurites outgrowth and promote survival of neurons and, hence, may be important in nerve regeneration through remyelination.
Interactions
Interleukin-6 has been shown to interact with interleukin-6 receptor, and glycoprotein 130.
There is considerable functional overlap and interaction between Substance P (SP), the natural ligand for the neurokinin type 1 receptor (NK1R, a mediator of immunomodulatory activity) and IL-6.
Role in disease
IL-6 stimulates the inflammatory and auto-immune processes in many diseases such as diabetes, atherosclerosis, depression, Alzheimer's Disease, systemic lupus erythematosus, multiple myeloma, prostate cancer, Behçet's disease, and rheumatoid arthritis.
Hence, there is an interest in developing anti-IL-6 agents as therapy against many of these diseases. The first such is tocilizumab, which has been approved for rheumatoid arthritis, Castleman's disease and systemic juvenile idiopathic arthritis. Others are in clinical trials.
Rheumatoid arthritis
The first FDA approved anti-IL-6 was for RA.
Cancer
Anti-IL-6 therapy was initially developed for treatment of autoimmune diseases, but due to the role of IL-6 in chronic inflammation, IL-6 blockade was also evaluated for cancer treatment. IL-6 was seen to have roles in tumor microenvironment regulation, production of breast cancer stem cell-like cells, metastasis through down-regulation of E-cadherin, and alteration of DNA methylation in oral cancer.
Advanced/metastatic cancer patients have higher levels of IL-6 in their blood. One example of this is pancreatic cancer, with noted elevation of IL-6 present in patients correlating with poor survival rates.
Enterovirus 71
High IL-6 levels are associated with the development of encephalitis in children and immunodeficient mouse models infected with Enterovirus 71; this highly contagious virus normally causes a milder illness called Hand, foot, and mouth disease but can cause life-threatening encephalitis in some cases. EV71 patients with a certain gene polymorphism in IL-6 also appear to be more susceptible to developing encephalitis.
Epigenetic modifications
IL-6 has been shown to lead to several neurological diseases through its impact on epigenetic modification within the brain. IL-6 activates the Phosphoinositide 3-kinase (PI3K) pathway, and a downstream target of this pathway is the protein kinase B (PKB) (Hodge et al., 2007). IL-6 activated PKB can phosphorylate the nuclear localization signal on DNA methyltransferase-1(DNMT1). This phosphorylation causes movement of DNMT1 to the nucleus, where it can be transcribed. DNMT1 recruits other DNMTs, including DNMT3A and DNMT3B, which, as a complex, recruit HDAC1. This complex adds methyl groups to CpG islands on gene promoters, repressing the chromatin structure surrounding the DNA sequence and inhibiting transcriptional machinery from accessing the gene to induce transcription. Increased IL-6, therefore, can hypermethylate DNA sequences and subsequently decrease gene expression through its effects on DNMT1 expression.
Schizophrenia
The induction of epigenetic modification by IL-6 has been proposed as a mechanism in the pathology of schizophrenia through the hypermethylation and repression of the GAD67 promoter. This hypermethylation may potentially lead to the decreased GAD67 levels seen in the brains of people with schizophrenia. GAD67 may be involved in the pathology of schizophrenia through its effect on GABA levels and on neural oscillations. Neural oscillations occur when inhibitory GABAergic neurons fire synchronously and cause inhibition of a multitude of target excitatory neurons at the same time, leading to a cycle of inhibition and disinhibition. These neural oscillations are impaired in schizophrenia, and these alterations may be responsible for both positive and negative symptoms of schizophrenia.
Depression and major depressive disorder
The epigenetic effects IL-6 have also been implicated in the pathology of depression. The effects of IL-6 on depression are mediated through the repression of brain-derived neurotrophic factor (BDNF) expression in the brain; DNMT1 hypermethylates the BDNF promoter and reduces BDNF levels. Altered BDNF function has been implicated in depression, which is likely due to epigenetic modification following IL-6 upregulation. BDNF is a neutrophic factor implicated in spine formation, density, and morphology on neurons. Downregulation of BDNF, therefore, may cause decreased connectivity in the brain. Depression is marked by altered connectivity, in particular between the anterior cingulate cortex and several other limbic areas, such as the hippocampus. The anterior cingulate cortex is responsible for detecting incongruences between expectation and perceived experience. Altered connectivity of the anterior cingulate cortex in depression, therefore, may cause altered emotions following certain experiences, leading to depressive reactions. This altered connectivity is mediated by IL-6 and its effect on epigenetic regulation of BDNF.
Additional preclinical and clinical data, suggest that Substance P [SP] and IL-6 may act in concert to promote major depression. SP, a hybrid neurotransmitter-cytokine, is co-transmitted with BDNF through paleo-spinothalamic circuitry from the periphery with collaterals into key areas of the limbic system. However, both IL6 and SP mitigate expression of BDNF in brain regions associated with negative affect and memory. SP and IL6 both relax tight junctions of the blood brain barrier, such that effects seen in fMRI experiments with these molecules may be a bidirectional mix of neuronal, glial, capillary, synaptic, paracrine, or endocrine-like effects. At the cellular level, SP is noted to increase expression of interleukin-6 (IL-6) through PI-3K, p42/44 and p38 MAP kinase pathways. Data suggest that nuclear translocation of NF-κB regulates IL-6 overexpression in SP-stimulated cells. This is of key interest as: 1) a meta-analysis indicates an association of major depressive disorder, C-reactive protein and IL6 plasma concentrations, 2) NK1R antagonists [five molecules] studied by 3 independent groups groups in over 2000 patients from 1998-2013 validate the mechanism as dose-related, fully effective antidepressant, with a unique safety profile. (see Summary of NK1RAs in Major Depression), 3) the preliminary observation that plasma concentrations of IL6 are elevated in depressed patients with cancer, and 4) selective NK1RAs may eliminate endogenous SP stress-induced augmentation of IL-6 secretion pre-clinically. These and many other reports suggest that a clinical study of a neutralizing IL-6 biological or drug based antagonist is likely warranted in patients with major depressive disorder, with or without co-morbid chronic inflammatory based illnesses; that the combination of NK1RAs and IL6 blockers may represent a new, potentially biomarkable approach to major depression, and possibly bipolar disorder.
The IL-6 antibody sirukumab is now undergoing clinical trials against major depressive disorder.
Asthma
Obesity is a known risk factor in the development of severe asthma. Recent data suggests that the inflammation associated with obesity, potentially mediated by the cytokine IL6, plays a role in causing poor lung function and increased risk for developing asthma exacerbations.
