Specialty rheumatology ICD-9-CM 446.4 MedlinePlus 000135 | ICD-10 M31.3 DiseasesDB 14057 eMedicine med/2401 | |
 | ||
Granulomatosis with polyangiitis (GPA), previously known as Wegener's granulomatosis (WG), is a systemic disorder that involves both granulomatosis and polyangiitis. It is a form of vasculitis (inflammation of blood vessels) that affects small- and medium-size vessels in many organs. Damage to the lungs and kidneys can be fatal. It requires long-term immunosuppression. The condition was originally named for Friedrich Wegener, who described the disease in 1936. As a response to Wegener's association with the German Nazi party, professional bodies and journals have replaced his name with a descriptive name. However, the older name is still often seen.
Contents
- Signs and symptoms
- Causes
- Pathophysiology
- Diagnosis
- Criteria
- Treatment
- Prognosis
- Epidemiology
- History
- References
Granulomatosis with polyangiitis is part of a larger group of vasculitic syndromes called systemic vasculitides or necrotizing vasculopathies, all of which feature an autoimmune attack by an abnormal type of circulating antibody termed ANCAs (antineutrophil cytoplasmic antibodies) against small and medium-size blood vessels. Apart from GPA, this category includes eosinophilic granulomatosis with polyangiitis (EGPA) and microscopic polyangiitis. Although GPA affects small- and medium-size vessels, it is formally classified as one of the small vessel vasculitides in the Chapel Hill system.
Signs and symptoms
Initial signs are extremely variable, and diagnosis can be severely delayed due to the nonspecific nature of the symptoms. In general, rhinitis is the first sign in most people.
Causes
Its causes are unknown, although microbes, such as bacteria and viruses, as well as genetics have been implicated in its pathogenesis.
Pathophysiology
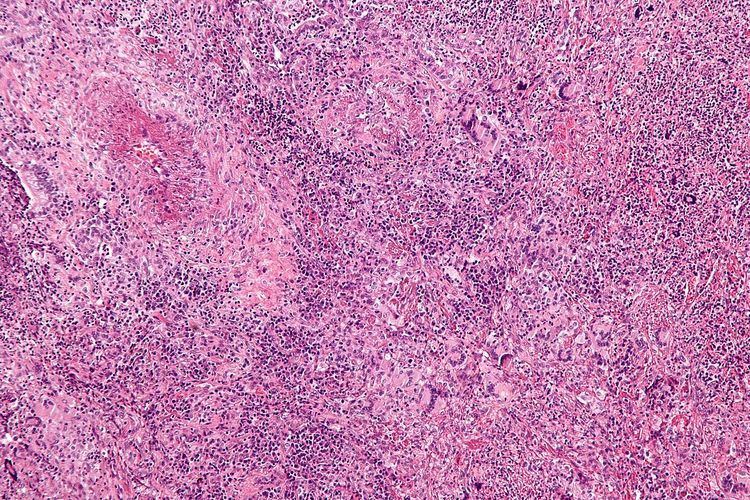
Inflammation with granuloma formation against a nonspecific inflammatory background is the classical tissue abnormality in all organs affected by GPA.
It is now widely presumed that the anti-neutrophil cytoplasmic antibodies (ANCAs) are responsible for the inflammation in GPA. The typical ANCAs in GPA are those that react with proteinase 3, an enzyme prevalent in neutrophil granulocytes.
In vitro studies have found that ANCAs can activate neutrophils, increase their adherence to endothelium, and induce their degranulation that can damage endothelial cells. In theory, this phenomenon could cause extensive damage to the vessel wall, in particular of arterioles.
Diagnosis
Granulomatosis with polyangiitis is usually suspected only when a person has had unexplained symptoms for a long period of time. Determination of Anti-neutrophil cytoplasmic antibodies (ANCAs) can aid in the diagnosis, but positivity is not conclusive and negative ANCAs are not sufficient to reject the diagnosis. Cytoplasmic-staining ANCAs that react with the enzyme proteinase 3 (cANCA) in neutrophils (a type of white blood cell) are associated with GPA.
If the person has kidney failure or cutaneous vasculitis, a biopsy is obtained from the kidneys. On rare occasions, thoracoscopic lung biopsy is required. On histopathological examination, a biopsy will show leukocytoclastic vasculitis with necrotic changes and granulomatous inflammation (clumps of typically arranged white blood cells) on microscopy. These granulomas are the main reason for the name granulomatosis with polyangiitis, although it is not an essential feature. Nevertheless, necrotizing granulomas are a hallmark of this disease. However, many biopsies can be nonspecific and 50% provide too little information for the diagnosis of GPA.
Criteria
In 1990, the American College of Rheumatology accepted classification criteria for GPA. These criteria were not intended for diagnosis, but for inclusion in randomized controlled trials. Two or more positive criteria have a sensitivity of 88.2% and a specificity of 92.0% of describing GPA.
According to the Chapel Hill Consensus Conference (CHCC) on the nomenclature of systemic vasculitis (1992), establishing the diagnosis of GPA demands:
Several investigators have compared the ACR and Chapel Hill criteria.
Treatment
The standard treatment for GPA is cyclophosphamide and high dose corticosteroids for remission induction and less toxic immunosuppressants like azathioprine, leflunomide, methotrexate or mycophenolate mofetil. Trimethoprim/sulfamethoxazole may also help prevent relapse. Rituximab may be substituted for cyclophosphamide in inducing remission. A systematic review of 84 trials examined the evidence for various treatments in GPA. Many trials include data on pooled groups of people with GPA and microscopic polyangiitis. In this review, cases are divided between localised disease, non-organ threatening, generalized organ-threatening disease and severe kidney vasculitis and immediately life-threatening disease.
Prognosis
Before modern treatments, the 2-year mortality was over 90% and average survival five months. Death usually resulted from uremia or respiratory failure.
With corticosteroids and cyclophosphamide, 5-year survival is over 80%. Long-term complications are common (86%), mainly chronic kidney failure, hearing loss and deafness.
Today, drug toxicity is managed more carefully and long-term remissions are possible. Some patients are able to lead relatively normal lives and remain in remission for 20+ years after treatment.
Epidemiology
The incidence is 10-20 cases per million per year. It is exceedingly rare in Japan and with African Americans.
History
Scottish otolaryngologist Peter McBride (1854–1946) first described the condition in 1897 in a BMJ article entitled "Photographs of a case of rapid destruction of the nose and face". Heinz Karl Ernst Klinger (born 1907) would add information on the anatomical pathology, but the full picture was presented by Friedrich Wegener (1907–1990), a German pathologist, in two reports in 1936 and 1939, leading to the name Wegener's granulomatosis or Wegener granulomatosis (English /ˈvɛɡənər/).
An earlier name for the disease was pathergic granulomatosis. The disease is still sometimes confused with lethal midline granuloma and lymphomatoid granulomatosis, both malignant lymphomas.
In 2006, Alexander Woywodt (Preston, United Kingdom) and Eric Matteson (Mayo Clinic, USA) investigated Wegener's past, and discovered that he was, at least at some point of his career, a follower of the Nazi regime. In addition, their data indicate that Wegener was wanted by Polish authorities and that his files were forwarded to the United Nations War Crimes Commission. Furthermore, Wegener worked in close proximity to the genocide machinery in Łódź. Their data raise serious concerns about Wegener's professional conduct. They suggest that the eponym should be abandoned and propose "ANCA-associated granulomatous vasculitis." The authors have since campaigned for other medical eponyms to be abandoned, too. In 2011, the American College of Rheumatology (ACR), the American Society of Nephrology (ASN) and the European League Against Rheumatism (EULAR) resolved to change the name to granulomatosis with polyangiitis.
