 | ||
The Bristol stool scale, Bristol stool chart (BSC), Bristol stool form scale, or BSF scale is a diagnostic medical tool designed to classify the form of human faeces into seven categories. It is used in both clinical and experimental fields. It is sometimes referred to in the UK as the Meyers scale.
Contents
Developed and proposed for the first time in England by Dr. Stephen Lewis and Dr. Ken Heaton at the University Department of Medicine, Bristol Royal Infirmary, it was suggested by the authors as a clinical assessment tool in 1997 in the journal Scandinavian Journal of Gastroenterology after a previous prospective study, conducted in 1992 on a sample of the population (838 men and 1,059 women), had shown an unexpected prevalence of defecation disorders related to the shape and type of stool. The authors of the former paper concluded that the form of the stool is a useful surrogate measure of colon transit time. That conclusion has since been challenged as having limited validity, and only in types 1 and 2 when the subject is not constipated; however, it remains in use as a research tool to evaluate the effectiveness of treatments for various diseases of the bowel, as well as a clinical communication aid.
The shape and consistency of stool depend with good statistical correlation from the time of permanence of the same in the colon.
The Bristol stool scale is part of the diagnostic triad for irritable bowel syndrome: pain/discomfort (quality and quantity), bowel habit (quality and quantity), and bloating (in women).
Interpretation of the scale
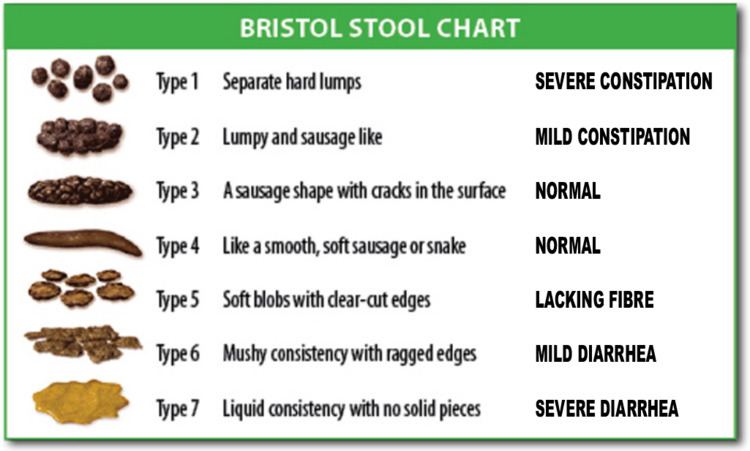
The seven types of stool are:
Types 1 and 2 indicate constipation, with 3 and 4 being the ideal stools (especially the latter), as they are easy to defecate while not containing excess liquid, and 5, 6 and 7 tending towards diarrhoea.
In the initial study it is interesting to note that, in the population examined in this scale, the type 1 and 2 stools were more prevalent in females, while the type 5 and 6 stools were more prevalent in males; furthermore, 80% of subjects who reported rectal tenesmus (urgency to defecate) had type 7. These and other data have allowed the scale to be validated.
The Bristol stool scale is also very sensitive to changes in intestinal transit time caused by medications, such as antidiarrhoeal loperamide or senna, anthraquinone substance with laxative effect.
Versions
The same scale is also validated in a Spanish version, and a version has also been designed and validated for paediatrics. More recently, in September 2011, a modified version of the scale was validated using a criterion of self-assessment for ages 6–8 years of age.
Diagnosis of IBS
Patients with IBS or irritable bowel syndrome typically report that they suffer with abdominal cramps and constipation. In some patients, chronic constipation is interspersed with brief episodes of diarrhoea; while a minority of patients with IBS have only diarrhoea. The presentation of symptoms is usually months or years and commonly patients consult different doctors, without great success, and doing various specialized investigations. It notices a strong correlation of the reported symptoms with stress; indeed diarrhoeal discharges are associated with emotional phenomena. IBS blood is present only if the disease is associated with haemorrhoids.
Research conducted on irritable bowel syndrome in the 2000s, faecal incontinence and the gastrointestinal complications of HIV have used the Bristol scale as a diagnostic tool easy to use; even in research which they lasted for 77 months.
Historically, this scale of assessment of the faeces has been recommended by the consensus group of Kaiser Permanente Medical Care Program (San Diego, California) for the collection of data on functional bowel disease (FBD).
More recently, according to the latest revision of the Rome III Criteria, six clinical manifestations of IBS can be identified:
These four identified subtypes correlate with the consistency of the stool, which can be determined by the Bristol stool scale.
In 2007, the Mayo Clinic College of Medicine in Rochester (United States), reported a piece of epidemiological research conducted on a population of 4,196 people living in Olmsted County (Minnesota), in which participants were asked to complete a questionnaire based on the Bristol stool scale.
The research results (see table) indicate that about 1 in 5 people have a slow transit (type 1 and 2 stools), while 1 in 12 has an accelerated transit (type 5 and 6 stools). Moreover, the nature of the stool is affected by age, sex, body mass index, by cholecystectomy and possible psychosomatic components (somatisation); there were no effects from factors such as smoking, alcohol, the level of education, a history of appendectomy or familiarity with gastrointestinal diseases civil, state, or the use of oral contraceptives.
Therapeutic evaluation
Several investigations correlate the Bristol stool scale in response to medications or therapies, in fact, in one study was also used to titrate the dose more finely than one drug (colestyramine) in subjects with diarrhoea and faecal incontinence.
In a randomised controlled study, the scale is used to study the response to two laxatives: Macrogol (polyethylene glycol) and psyllium (Plantago psyllium and other species of the same genus) of 126 male and female patients for a period of 2 weeks of treatment; failing to show the most rapid response and increased efficiency of the former over the latter. In the study, they were measured as primary outcomes: the number weekly bowel movements, stool consistency according to the types of the Bristol stool scale, time to defecation, the overall effectiveness, the difficulty in defecating and stool consistency.
From 2010, several clinical studies have used the scale as a diagnostic tool validated for recognition and evaluation of response to various treatments, pharmacological and no, different, such as: probiotics, moxicombustion, laxatives in the elderly, preparing Ayurvedic poly-phytotherapy filed TLPL/AY, psyllium, mesalazine, methylnaltrexone, and oxycodone/naloxone. Or to assess the response to physical activity in athletes.
