Latin nodus sinuatrialis MeSH A07.541.409.819 | Acronym(s) SAN; SA node Dorlands/Elsevier 12577255 | |
 | ||
Artery Sinoatrial nodal artery | ||
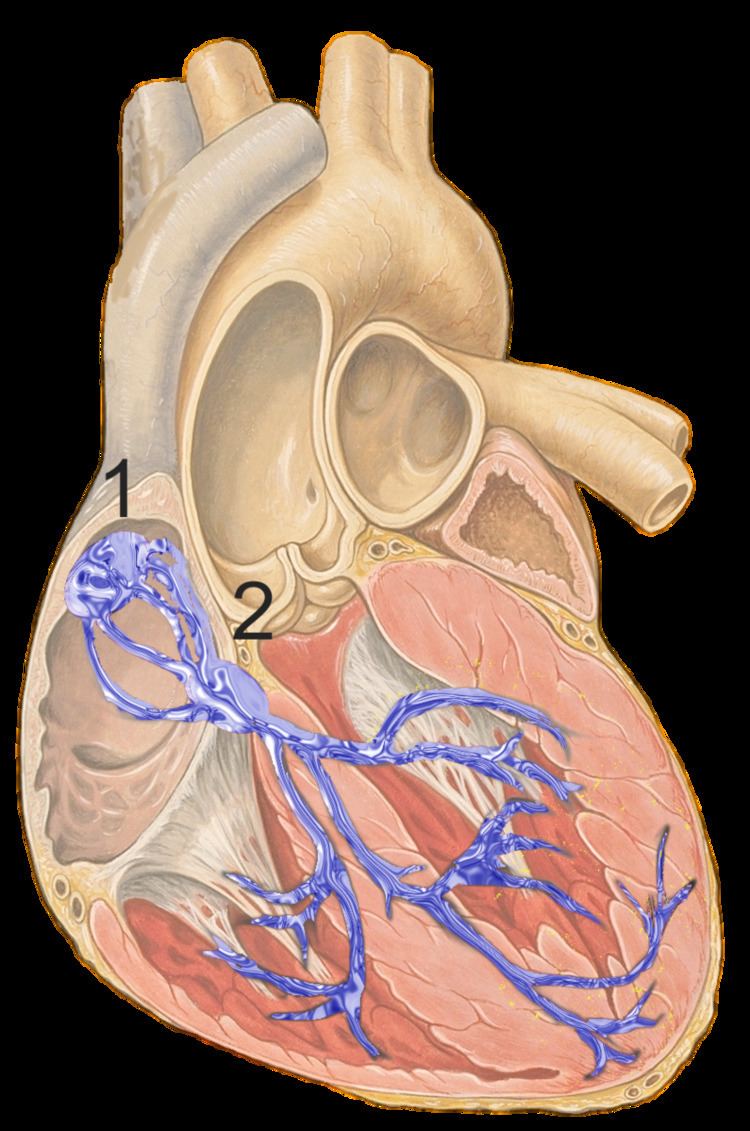
The sinoatrial node (SAN; also known as sinus node) is a group of cells located in the wall of the right atrium of the heart. These cells have the ability to spontaneously produce an electrical impulse (action potential; see below for more details), that travels through the heart via the electrical conduction system (see figure 1) causing it to contract. In a healthy heart, the SAN continuously produces action potential, setting the rhythm of the heart and so is known as the hearts natural pacemaker. The rate of action potential production (and therefore the heart rate) is influenced by nerves that supply it.
Contents
Structure
The sinoatrial node is a banana-shaped structure that varies in size, usually between 10-30millimeter (mm) long, 5-7mm wide and 1-2mm deep (1millimeter= 0.001meter).
Location
The SAN is located in the wall (myocardium) of the right atrium, laterally to the entrance of the superior vena cava in a region called the sinus venarum (hence sino- + atrial). It is positioned roughly between a groove called the crista terminalis located on the external surface of the heart and the corresponding sulcus terminalis, on the internal surface. These grooves run between the entrance of the superior vena cava and the inferior vena cava
Microanatomy
The cells of the SAN are spread out within a mesh of connective tissue, containing nerves, blood vessels, collagen and fat. Immediately surrounding the SAN cells, are paranodal cells. These cells have structures intermediate between that of the SAN cells and the rest of the atrium. The connective tissue, along with the paranodal cells insulate the SAN from the rest of the atrium preventing the electrical activity of the atrial cells from affecting the SAN cells. The SAN cells are smaller and paler than the surrounding atrial cells, with the average cell being around 8micrometers in diameter, and 20-30 micrometers in length (1 micrometer= 0.000001 meter). Unlike the atrial cells, SAN cells contain fewer mitochondria (the power plant of the cell), have fewer myofibers (contractile machinery of the cell) and a smaller sarcoplasmic reticulum (calcium store unit, that releases calcium for contraction). This means that the SAN cells are less equipped to contract, compared to the atrial and ventricular cells.
Action potentials pass from one cardiac cell, to the next through pores known as gap junctions. These gap junctions are made of proteins called connexins. There are fewer gap junctions within the SAN and they are smaller in size. This is again important in insulating the SAN from the surrounding atrial cells.
Blood supply
The SA Node receives its blood supply from the sinoatrial node artery. This blood supply, however, can differ hugely between individuals. For example, in most humans, this is a single artery, although in some cases there have been either 2 or 3 sinoatrial node arteries supplying the SAN. Also, the SAN artery, mainly originates as a branch of an artery called the right coronary artery, however in some individuals, it has arisen from the circumflex artery, which is a branch of the left coronary artery. Finally, the SAN artery commonly passes behind the superior vena cava, before reaching the SAN, however in some instances it passes in front. Despite these many differences, there doesn’t appear to be any advantage how many sinoatrial nodal arteries an individual has, or where they originate from
Venous drainage
There are no large veins that drain blood away from the SAN. Instead smaller venules, drain the blood directly into the right atrium.
Pacemaking
The main role of a sinoatrial node cell is to initiate action potentials, so that it can pass throughout the heart and cause contraction. An action potential is a change in voltage(membrane potential) across the membrane of the cell, produced by the movement of charged atoms (ions). Non-pacemaker cells (including the ventricular and atrial cells) have a period, immediately after an action potential, where the membrane potential remains relatively constant, this is known as a resting membrane potential. This resting phase (see cardiac action potential, phase 4) ends when another action potential reaches the cell. This produces a positive change in membrane potential (known as depolarisation), which initiates the start of the next action potential. Pacemaker cells, however, don’t have this resting phase. Instead, immediately after one action potential, the membrane potential of these cells begins to depolarise again automatically, this is known as the pacemaker potential. Once the pacemaker potential reaches a set value, known as the threshold value, it then produces an action potential. Other cells within the heart (including the purkinje fibers and atrioventricular node; AVN) can also initiate action potentials, however they do so at a slower rate and therefore, if the SAN is working, it usually beats the AVN to it.
Outlined below are the 3 phases of a sinoatrial node action potential. In the ventricular action potential, there are 5 phases (labelled 0-4), however pacemaker action potentials don’t have an obvious phase 1 or 2.
Phase 4
This phase is also known as the pacemaker potential. Immediately following an action potential, when the membrane potential is very negative (it is hyperpolarised) the voltage slowly begins to increase. This is initially due to the closing of potassium channels, which reduces the flow of potassium ions (Ik) out of the cell (see phase 3, below). Alongside the deactivation of the potassium channels, channels known as hyperpolarisation-activated cyclic nucleotide–gated (HCN) channels, are activated. Activation of these channels at very negative membrane potential is an unusual property for ion channels, therefore the flow of sodium (Na+) and some potassium (K+) through the activated HCN channel is referred to as a funny current (If). This funny current causes the membrane potential of the cell to gradually increase, as the positive charge (Na+ and K+) is flowing into the cell. Another mechanism involved in pacemaker potential is known as the calcium clock. Here, calcium is released spontaneously from the sarcoplasmic reticulum (a calcium store) into the cell, this is known as a spontaneous Ca2+ spark. This in-crease in calcium within the cell then activates a sodium-calcium exchanger (NCX), which removes one Ca2+ from the cell, and exchanges it for 3 Na+ into the cell (therefore removing a charge of +2 from the cell, but allowing a charge of +3 to enter the cell) therefore in-creasing the membrane potential. The calcium is later pumped back into the cell via calcium channels located on the cell membrane and SR membrane. The increase in membrane potential produced by these mechanisms, activates T-type calcium channels and then L-type calcium channels (which open very slowly). These channels allow a flow of calcium ions (Ca2+) into the cell, making the membrane potential more positive.
Phase 0
This is the depolarisation phase. When the membrane potential reaches a threshold value (around -20 to -50 mV), it begins to rapidly depolarise (become more positive). This is mainly due to the flow of Ca2+ through the L-type calcium channels, which are now fully open. During this stage the T-type calcium channels and HCN channels deactivate.
Phase 3
This phase is the repolarisation phase. This occurs due to the inactivation of the L-type calcium channels (preventing the movement of Ca2+ into the cell), and the activation of potassium channels, which allows the flow of K+ out of the cell, making the membrane potential more negative.
Nerve supply
Heart rate depends on the rate at which the sinoatrial node produces action potentials. At rest, heart rate is between 60 and 100 beats per minute. This is a result of the activity of two sets of nerves, one acting to slow down action potential production (these are parasympathetic nerves) and the other acting to speed up action potential production (sympathetic nerves).
The sympathetic nerves begin in the thoracic region of the spinal cord (in particular T1-T4). These nerves release a neurotransmitter (protein) called noradrenaline (NA). This binds to a receptor on the SAN membrane, called a beta-1adrenoceptor. Binding of NA to this receptor activates a G-protein (in particular a Gs-Protein, S for stimulatory) which initiates a series of reactions (known as the cAMP pathway) that results in the production of a molecule called cyclic adenosinemonophosphate (cAMP). This cAMP binds to the HCN channel (see above). Binding of cAMP to the HCN, increases the flow of Na+ and K+ into the cell, speeding up the pacemaker potential, so producing action potentials at a quicker rate, and increaing heart rate. An increase in heart rate is known as positive chronotropy.
The parasympathetic nerves supplying the SAN (in particular the Vagus nerves) originate in the brain. These nerves release a neurotransmitter called acetylcholine (ACh). ACh binds to a receptor called an M2 muscarinic receptor, located on the SAN membrane. Activation of this M2 receptor, then activates a protein called a G-protein (in particular Gi protein, i for inhibitory). Activation of this G-protein, blocks the cAMP pathway, reducing its effects, therefore inhibiting sympathetic activity and slowing action potential production. As well as this, the G-protein also activates a potassium channel, which allows K+ to flow out of the cell, making the membrane potential more negative and slowing the pacemaker potential, therefore decreasing the rate of action potential production and therefore decreasing heart rate. A decrease in heart rate is known as negative chronotropy.
The first cell to produce the action potential in the SAN isn’t always the same, this is known as pacemaker shift. In certain species of animals, for example, in dogs, a superior shift (i.e. the cell that produces the fastest action potential in the SAN is higher than previously) usually produced an increased heart rate whereas an inferior shift (i.e. the cell producing the fastest action potential within the SAN is further down than previously) produced a decreased heart rate.
Clinical significance
Sinus node dysfunction describes an irregular heartbeat caused by faulty electrical signals of the heart. When the heart's sinoatrial node is defective, the heart’s rhythms become abnormal – typically too slow or exhibiting pauses in its function or a combination, and very rarely faster than normal.
Blockage of the arterial blood supply to the SA node (most commonly due to a myocardial infarction or progressive coronary artery disease) can therefore cause ischaemia and cell death in the SA node. This can disrupt the electrical pacemaker function of the SA node, and can result in sick sinus syndrome.
If the SA node does not function, or the impulse generated in the SA node is blocked before it travels down the electrical conduction system, a group of cells further down the heart will become its pacemaker.
History
The sinoatrial node was first discovered by a young medical student, Martin Flack, in the heart of a mole, whilst his mentor, Sir Arthur Keith, was on a bicycle ride with his wife. They made the discovery in a makeshift laboratory set up in a picturesque farmhouse in Kent, England, called Mann's Place. Their discovery was published in 1907.
