Trade names Inderal License data US FDA: Propranolol ATC code C07AA05 (WHO) Bioavailability 26% Pubchem 4946 | AHFS/Drugs.com Monograph Molar mass 259.34 g/mol CAS ID 525-66-6 | |
 | ||
Pregnancycategory AU: CUS: C (Risk not ruled out) | ||
The migraine guy propranolol
Propranolol is a medication of the beta blocker type. It is used to treat high blood pressure, a number of types of irregular heart rate, thyrotoxicosis, capillary hemangiomas, performance anxiety, and essential tremors. It is used to prevent migraine headaches, and to prevent further heart problems in those with angina or previous heart attacks. It can be taken by mouth or by injection into a vein. The formulation that is taken by mouth comes in short acting and long acting versions. Propranolol appears in the blood after 30 minutes and has a maximum effect between 60 and 90 minutes when taken by mouth.
Contents
- The migraine guy propranolol
- Propranolol
- Medical uses
- Cardiovascular
- Psychiatric
- PTSD and phobias
- Others
- Adverse effects
- Precautions and contraindications
- Pregnancy and lactation
- Overdose
- Interactions
- Pharmacokinetics
- Mechanism of action
- History
- Society and culture
- Brand names
- Research
- References
Common side effects include nausea, abdominal pain, and constipation. It should not be used in those with an already slow heart rate and most of those with heart failure. Quickly stopping the medication in those with coronary artery disease may worsen symptoms. It may worsen the symptoms of asthma. Greater care is recommended in those with liver or kidney problems. Propranolol may cause harmful effects in the baby if taken during pregnancy. Its use during breastfeeding is probably safe, but the baby should be monitored for side effects. It is a non-selective beta blocker which works by blocking β-adrenergic receptors.
Propranolol was discovered in 1964. It is on the World Health Organization's List of Essential Medicines, the most effective and safe medicines needed in a health system. Propranolol is available as a generic medication. The wholesale cost in the developing world is between 0.24 and 2.16 USD per month as of 2014. In the United States it costs about 15 USD per month at a typical dose.
Propranolol
Medical uses
Propranolol is used for treating various conditions, including:
Cardiovascular
While once a first-line treatment for hypertension, the role for beta blockers was downgraded in June 2006 in the United Kingdom to fourth-line, as they do not perform as well as other drugs, particularly in the elderly, and evidence is increasing that the most frequently used beta blockers at usual doses carry an unacceptable risk of provoking type 2 diabetes.
Propranolol is not recommended for the treatment of hypertension by the Eighth Joint National Committee (JNC 8) because a higher rate of the primary composite outcome of cardiovascular death, myocardial infarction, or stroke compared to an angiotensin receptor blocker was noted in one study.
Psychiatric
It is occasionally used to treat performance anxiety. Evidence to support the use in other anxiety disorders is poor. Some experimentation has been conducted in other psychiatric areas:
PTSD and phobias
Propranolol is being investigated as a potential treatment for PTSD. Propranolol works to inhibit the actions of norepinephrine, a neurotransmitter that enhances memory consolidation. Individuals given propranolol immediately after trauma experienced fewer stress-related symptoms and lower rates of PTSD than respective control groups who did not receive the drug. Due to the fact that memories and their emotional content are reconsolidated in the hours after they are recalled/re-experienced, propranolol can also diminish the emotional impact of already formed memories; for this reason, it is also being studied in the treatment of specific phobias, such as arachnophobia, dental fear, and social phobia.
Ethical and legal questions have been raised surrounding the use of propranolol-based medications for use as a "memory damper", including: altering memory-recalled evidence during an investigation, modifying behavioral response to past (albeit traumatic) experiences, the regulation of these drugs, and others. However, Hall and Carter have argued that many such objections are "based on wildly exaggerated and unrealistic scenarios that ignore the limited action of propranolol in affecting memory, underplay the debilitating impact that PTSD has on those who suffer from it, and fail to acknowledge the extent to which drugs like alcohol are already used for this purpose."
Others
Propranolol may be used to treat severe infantile hemangiomas (IHs). This treatment shows promise as being superior to corticosteroids when treating IHs. Extensive clinical case evidence and a small controlled trial support its efficacy.
Adverse effects
Due to the high penetration across the blood–brain barrier, lipophilic beta blockers such as propranolol and metoprolol are more likely than other less lipophilic beta blockers to cause sleep disturbances such as insomnia and vivid dreams, and nightmares. Dreaming (rapid eye movement sleep, REM) was reduced and increased awakening.
Adverse drug reactions associated with propranolol therapy are similar to other lipophilic beta blockers.
Precautions and contraindications
Propranolol should be used with caution in people with:
Propranolol is contraindicated in patients with:
Pregnancy and lactation
Propranolol, like other beta blockers, is classified as pregnancy category C in the United States and ADEC category C in Australia. β-blocking agents in general reduce perfusion of the placenta which may lead to adverse outcomes for the neonate, including pulmonary or cardiac complications, or premature birth. The newborn may experience additional adverse effects such as hypoglycemia and bradycardia.
Most β-blocking agents appear in the milk of lactating women. However, propranolol is highly bound to proteins in the bloodstream and is distributed into breast milk at very low levels. These low levels are not expected to pose any risk to the breastfeeding infant, and the American Academy of Pediatrics considers propranolol therapy "generally compatible with breastfeeding".
Overdose
In overdose propranolol is associated with seizures. Cardiac arrest may occur in propranolol overdose due to sudden ventricular arrhythmias, or cardiogenic shock which may ultimately culminate in bradycardic PEA. Therefore, propranolol should be used with extreme caution in depressed or atypically depressed patients with possible suicidal ideation.
Interactions
Since beta blockers are known to relax the cardiac muscle and to constrict the smooth muscle, beta-adrenergic antagonists, including propranolol, have an additive effect with other drugs which decrease blood pressure, or which decrease cardiac contractility or conductivity. Clinically significant interactions particularly occur with:
Pharmacokinetics
Propranolol is rapidly and completely absorbed, with peak plasma levels achieved about 1–3 hours after ingestion. Coadministration with food appears to enhance bioavailability. Despite complete absorption, propranolol has a variable bioavailability due to extensive first-pass metabolism. Hepatic impairment therefore increases its bioavailability. The main metabolite 4-hydroxypropranolol, with a longer half-life (5.2–7.5 hours) than the parent compound (3–4 hours), is also pharmacologically active.
Propranolol is a highly lipophilic drug achieving high concentrations in the brain. The duration of action of a single oral dose is longer than the half-life and may be up to 12 hours, if the single dose is high enough (e.g., 80 mg). Effective plasma concentrations are between 10 and 100 mg/l. Toxic levels are associated with plasma concentrations above 2000 mg/l.
Mechanism of action
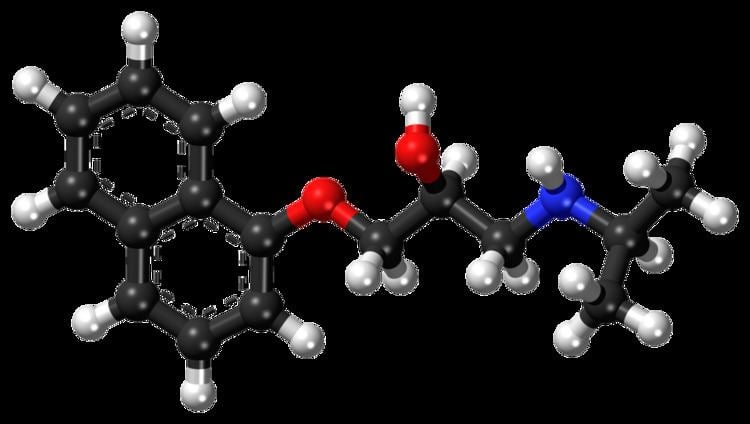
Propranolol is classified as a non-cardioselective sympatholytic beta blocker that crosses the blood–brain barrier. It is lipid soluble and also has sodium channel blocking effects. Propranolol is a non-selective beta blocker; that is, it blocks the action of epinephrine (adrenaline) and norepinephrine (noradrenaline) at both β1- and β2-adrenergic receptors. It has little intrinsic sympathomimetic activity, but has strong membrane stabilizing activity (only at high blood concentrations, e.g. overdose). Propranolol is able to cross the blood–brain barrier and exert effects in the central nervous system in addition to its peripheral activity.
In addition to blockade of adrenergic receptors, propranolol has weak inhibitory effects on the norepinephrine transporter and/or weakly stimulates norepinephrine release (i.e., the concentration of norepinephrine is increased in the synapse). Since propranolol blocks β-adrenoceptors, the increase in synaptic norepinephrine only results in α-adrenoceptor activation, with the α1-adrenoceptor being particularly important for effects observed in animal models. Therefore, it can be looked upon as a weak indirect α1-adrenoceptor agonist in addition to potent β-adrenoceptor antagonist. In addition to its effects on the adrenergic system, there is evidence that indicates that propranolol may function as an antagonist of certain serotonin receptors, namely the 5-HT1A and 5-HT1B receptors.
Both enantiomers of propranolol have a local anesthetic (topical) effect, which is normally mediated by blockade of voltage-gated sodium channels. Studies have demonstrated propranolol's ability to block cardiac, neuronal, and skeletal voltage-gated sodium channels, accounting for its known membrane stabilizing effect and antiarrhythmic and other central nervous system effects.
History
British scientist James W. Black developed propranolol in the 1960s. In 1988, he was awarded the Nobel Prize in Medicine for this discovery. Propranolol was inspired by the early β-adrenergic antagonists dichloroisoprenaline and pronethalol. The key difference, which was carried through to essentially all subsequent beta blockers, was the inclusion of an oxymethylene group (-O-CH2-) between the aryl and ethanolamine moieties of pronethalol, greatly increasing the potency of the compound. This also apparently eliminated the carcinogenicity found with pronethalol in animal models.
Newer, more cardio-selective beta blockers (such as bisoprolol, nebivolol, carvedilol, or metoprolol) are now used in the treatment of hypertension.
Society and culture
In a 1987 study by the International Conference of Symphony and Opera Musicians, 27% of interviewed members admitted to using beta blockers such as propranolol for musical performances. For about 10–16% of performers, their degree of stage fright is considered pathological. Propranolol is used by musicians, actors, and public speakers for its ability to treat anxiety symptoms activated by the sympathetic nervous system.
Brand names
Original propranolol was marketed in 1965 under the brand name Inderal and manufactured by ICI Pharmaceuticals (now AstraZeneca). Propranolol is also marketed under brand names Avlocardyl, Deralin, Dociton, Inderalici, InnoPran XL, Sumial, Anaprilin, and Bedranol SR (Sandoz). In India it is marketed under brand names such as Ciplar and Ciplar LA by Cipla. Hemangeol, a 4.28 mg/mL solution of propranolol, is indicated for the treatment of proliferating infantile hemangioma.
Research
In 2015, a trial in women with epithelial ovarian cancer showed that the intake of a non-selective β-blocker was associated with a longer survival compared to a β1-selective β-blocker or no β-blocker. Currently, an interventional study is being conducted at the M.D. Anderson Cancer Center to assess the feasibility of a non-selective β-blocker plus standard chemotherapy (paclitaxel and carboplatin or possibly docetaxel) to treat ovarian cancer.
