Entrez 5741 | Ensembl ENSG00000152266 | |
 | ||
External IDs MGI: 97799 HomoloGene: 266 GeneCards: PTH | ||
Parathyroid hormone
Parathyroid hormone (PTH), also called parathormone or parathyrin, is a hormone secreted by the parathyroid glands that is important in bone remodeling, which is an ongoing process in which bone tissue is alternately resorbed and rebuilt over time. It essentially increases blood calcium levels. The bones act as a (metaphorical) "bank of calcium" from which the body can make "withdrawals" as needed to keep the amount of calcium in the blood at appropriate levels despite the ever-present challenges of metabolism, stress, and nutritional variations. PTH is "a key that unlocks the bank vault" to remove the calcium. In consequence, PTH is vital to health, and health problems that yield too little or too much PTH (such as hypoparathyroidism, hyperparathyroidism, or paraneoplastic syndromes) can wreak havoc in the form of bone disease, hypocalcaemia, and hypercalcaemia.
Contents
- Parathyroid hormone
- Hyperparathyroidism nursing symptoms pathophysiology nclex parathyroid hormone gland disorders
- Structure
- Regulation of serum calcium
- Regulation of serum phosphate
- Vitamin D synthesis
- Interactive pathway map
- Regulation of PTH secretion
- Stimulators
- Inhibitors
- Clinical significance
- Measurement
- Model organisms
- References
PTH is secreted by the chief cells of the parathyroid glands as a polypeptide containing 84 amino acids, which is a prohormone; effective hormone-receptor interaction requires solely the 34-N-terminal amino acids. While PTH acts to increase the concentration of ionic calcium (Ca2+) in the blood, calcitonin, a hormone produced by the parafollicular cells (C cells) of the thyroid gland, acts to decrease ionic calcium concentration. PTH essentially acts to increase the concentration of calcium in the blood by acting upon the parathyroid hormone 1 receptor, which is present at high levels in bone and kidney, and the parathyroid hormone 2 receptor, which is present at high levels in the central nervous system, pancreas, testis, and placenta. PTH half-life is approximately 4 minutes. It has a molecular mass of approximately 9500 Da.
Hyperparathyroidism nursing symptoms pathophysiology nclex parathyroid hormone gland disorders
Structure
hPTH-(1-34) crystallizes as a slightly bent, long helical dimer. Analysis reveals that the extended helical conformation of hPTH-(1-34) is the likely bioactive conformation. The N-terminal fragment 1-34 of parathyroid hormone (PTH) has been crystallized and the structure has been refined to 0.9 Å resolution.
Regulation of serum calcium
Parathyroid hormone regulates serum calcium through its effects on bone, kidney, and the intestine:
In bone, PTH enhances the release of calcium from the large reservoir contained in the bones. Bone resorption is the normal destruction of bone by osteoclasts, which are indirectly stimulated by PTH. Stimulation is indirect since osteoclasts do not have a receptor for PTH; rather, PTH binds to osteoblasts, the cells responsible for creating bone. Binding stimulates osteoblasts to increase their expression of RANKL and inhibits their secretion of Osteoprotegerin (OPG). Free OPG competitively binds to RANKL as a decoy receptor, preventing RANKL from interacting with RANK, a receptor for RANKL. The binding of RANKL to RANK (facilitated by the decreased amount of OPG available for binding the excess RANKL) stimulates these osteoclast precursors to fuse, forming new osteoclasts, which ultimately enhances bone resorption.
In the kidney, approximately 250 mmol of calcium ions are filtered into the glomerular filtrate per day. Most of this (245 mmol/d) is reabsorbed from the tubular fluid, leaving about 5 mmol/d to be excreted in the urine. This reabsorption occurs throughout the tubule (most, 60-70%, of it in the proximal tubule), except in the thin segment of the loop of Henle. Circulating parathyroid hormone only influences the reabsorption that occurs in the distal tubules and the renal collecting ducts (but see Foot Note). A more important effect of PTH on the kidney is, however, its inhibition of the reabsorption of phosphate (HPO42−) from the tubular fluid, resulting in a decrease in the plasma phosphate concentration. Phosphate ions form water-insoluble salts with calcium. Thus, a decrease in the phosphate concentration of the blood plasma (for a given total calcium concentration) increases the amount of calcium that is ionized. A third important effect of PTH on the kidney is its stimulation of the conversion of 25-hydroxy vitamin D into 1,25-dihydroxy vitamin D (calcitriol), which is released into the circulation. This latter form of vitamin D is the active hormone which stimulates calcium uptake from the intestine.
In the intestine, via kidney, PTH enhances the absorption of calcium in the intestine by increasing the production of activated vitamin D. Vitamin D activation occurs in the kidney. PTH up-regulates 25-hydroxyvitamin D3 1-alpha-hydroxylase, the enzyme responsible for 1-alpha hydroxylation of 25-hydroxy vitamin D, converting vitamin D to its active form (1,25-dihydroxy vitamin D). This activated form of vitamin D increases the absorption of calcium (as Ca2+ ions) by the intestine via calbindin.
PTH was one of the first hormones to be shown to use the G-protein, adenylyl cyclase second messenger system.
Regulation of serum phosphate
PTH reduces the reabsorption of phosphate from the proximal tubule of the kidney, which means more phosphate is excreted through the urine.
However, PTH enhances the uptake of phosphate from the intestine and bones into the blood. In the bone, slightly more calcium than phosphate is released from the breakdown of bone. In the intestines, absorption of both calcium and phosphate is mediated by an increase in activated vitamin D. The absorption of phosphate is not as dependent on vitamin D as is that of calcium. The end result of PTH release is a small net drop in the serum concentration of phosphate.
Vitamin D synthesis
PTH increases the activity of 1-α-hydroxylase enzyme, which converts 25-hydroxycholecalciferol, the major circulating form of inactive vitamin D, into 1,25-dihydroxycholecalciferol, the active form of vitamin D, in the kidney.
Interactive pathway map
Click on genes, proteins and metabolites below to link to respective articles.
Regulation of PTH secretion
Secretion of parathyroid hormone is determined chiefly by serum ionized calcium concentration through negative feedback. Calcium-sensing receptors located on parathyroid cells. PTH is secreted when [Ca2+] is decreased (Calcitonin is secreted when serum calcium levels are elevated). The G-protein coupled calcium receptors bind extracellular calcium and may be found on the surface on a wide variety of cells distributed in the brain, heart, skin, stomach, C cells, and other tissues. In the parathyroid gland, high concentrations of extracellular calcium result in activation of the Gq G-protein coupled cascade through the action of phospholipase C. This hydrolyzes phosphatidylinositol 4,5-bisphosphate (PIP2) to liberate intracellular messengers IP3 and diacylglycerol (DAG). Ultimately, these two messengers result in a release of calcium from intracellular stores into the cytoplasmic space. Hence a high extracellular calcium concentration leads to an increase in the cytoplasmic calcium concentration. In contrast to the mechanism that most secretory cells use, this high cytoplasmic calcium concentration inhibits the fusion of vesicles containing granules of preformed PTH with the membrane of the parathyroid cell, and thus inhibits release of PTH.
In the parathyroids, magnesium serves this role in stimulus-secretion coupling. A mild decrease in serum magnesium levels stimulates the resorptive activity PTH has on the kidneys. Severe Hypomagnesemia inhibits PTH secretion and also causes resistance to PTH, leading to a form of hypoparathyroidism that is reversible.
Stimulators
Inhibitors
Clinical significance
Hyperparathyroidism, the presence of excessive amounts of parathyroid hormone in the blood, occurs in two very distinct sets of circumstances. Primary hyperparathyroidism is due to autonomous, abnormal hypersecretion of PTH from the parathyroid gland, while secondary hyperparathyroidism is an appropriately high PTH level seen as a physiological response to hypocalcaemia. A low level of PTH in the blood is known as hypoparathyroidism and is most commonly due to damage to or removal of parathyroid glands during thyroid surgery.
There are a number of rare but well-described genetic conditions affecting parathyroid hormone metabolism, including pseudohypoparathyroidism, familial hypocalciuric hypercalcaemia, and autosomal dominant hypercalciuric hypocalcaemia. In osteoporotic women, administration of an exogenous parathyroid hormone analogue (teriparatide, by daily injection) superimposed on estrogen therapy produced increases in bone mass and reduced vertebral and nonvertebral fractures by 45 to 65%.
Measurement
PTH can be measured in the blood in several different forms: intact PTH; N-terminal PTH; mid-molecule PTH, and C-terminal PTH, and different tests are used in different clinical situations.
The average PTH level is 8–51 pg/mL. Normal total plasma calcium level ranges from 8.5 to 10.2 mg/dL (2.12 mmol/L to 2.55 mmol/L).
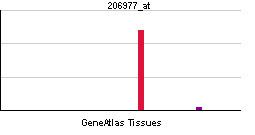
Model organisms
Model organisms have been used in the study of PTH function. A conditional knockout mouse line called Pthtm1a(EUCOMM)Wtsi was generated at the Wellcome Trust Sanger Institute. Male and female animals underwent a standardized phenotypic screen to determine the effects of deletion. Additional screens performed: - In-depth immunological phenotyping
