ICD-10 I33 MedlinePlus 000681 | ICD-9-CM 421.0-421.1 | |
 | ||
Specialty Cardiology, infectious disease | ||
Infective endocarditis is a form of endocarditis. It is an inflammation of the inner tissues of the heart, the endocardium, usually of the valves. It is caused by infectious agents, or pathogens, which are largely bacterial but a few other organisms can also be responsible. Before the age of modern antibiotics it was almost universally fatal.
Contents
- Duration
- Culture results
- Heart side
- Infection setting
- Valve type
- Signs and symptoms
- Cause
- Bacterial
- Fungal
- Risk factors
- Dental operations
- Pathogenesis
- Diagnosis
- Echocardiography
- Modified Duke criteria
- Major criteria
- Minor criteria
- Risk
- Prevention
- Treatment
- Epidemiology
- References
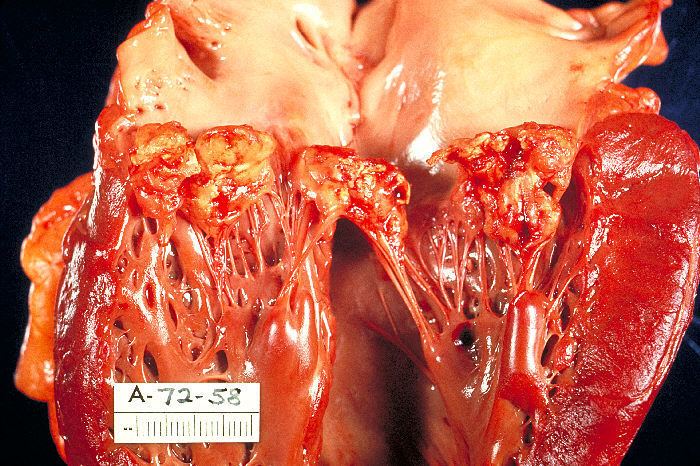
The valves of the heart do not receive any dedicated blood supply. As a result, defensive immune system mechanisms (such as white blood cells) cannot directly reach the valves via the bloodstream. If an organism (such as bacteria) attaches to a valve surface and forms a vegetation, the host's immune response is blunted. The lack of blood supply to the valves also has implications for treatment, since drugs also have difficulty reaching the infected area.
Normally, blood flows smoothly through these valves. If they have been damaged — from rheumatic fever, for example — the risk of bacterial attachment is increased.
Duration
Historically, infective endocarditis has been clinically divided into acute and subacute presentations (because untreated patients tended to live longer with the subacute as opposed to the acute form). This classifies both the rate of progression and severity of disease.
This classification is now discouraged, because the ascribed associations (in terms of organism and prognosis) were not strong enough to be relied upon clinically. The terms short incubation (meaning less than about six weeks), and long incubation (greater than about six weeks) are preferred.
Culture results
Infective endocarditis may also be classified as culture-positive or culture-negative. By far the most common cause of a "culture-negative" endocarditis is prior administration of antibiotics.
Sometimes microorganisms can take a longer period of time to grow in the culture media, such organisms are said to be fastidious because they have demanding growth requirements. Some examples include pathogens like Aspergillus species, Brucella species, Coxiella burnetii, Chlamydia species, and HACEK bacteria. Due to delay in growth and identification in these cases, patients may be erroneously classified as "culture-negative" endocarditis.
Heart side
Endocarditis can also be classified by the side of the heart affected:
Infection setting
Another form of endocarditis is healthcare-associated endocarditis when the infecting organism is believed to be transmitted in a health care setting like hospital, dialysis unit or a residential nursing home. Nosocomial endocarditis is a form of healthcare associated endocarditis in which the infective organism is acquired during stay in a hospital and it is usually secondary to presence of intravenous catheters, total parenteral nutrition lines, pacemakers, etc.
Valve type
Finally, the distinction between native-valve endocarditis and prosthetic-valve endocarditis is clinically important. Prosthetic valve endocarditis can be early (< 60 days of valvular surgery), intermediate (60 days to 1 year) or late (> 1 year following valvular surgery).
Prosthetic valve endocarditis is commonly caused by Staphylococcus epidermidis as it is capable of growing as a biofilm on plastic surfaces.
Signs and symptoms
Cause
Many microorganisms can cause infective endocarditis. These are generally isolated by blood culture, where the patient's blood is removed, and any growth is noted and identified. The term bacterial endocarditis (BE) commonly is used, reflecting the fact that most cases of IE are due to bacteria; however, infective endocarditis (IE) has become the preferred term.
Bacterial
Staphylococcus aureus followed by Streptococci of the viridans group and coagulase negative Staphylococci are the three most common organisms responsible for infective endocarditis. Other Streptococci and Enterococci are also a frequent cause of infective endocarditis. HACEK group of microorganisms and fungi are seen less frequently in North America.
Viridans Alpha-hemolytic streptococci, that are present in the mouth are the most frequently isolated microorganisms when the infection is acquired in a community setting. In contrast, Staphylococcus blood stream infections are frequently acquired in a health care setting where they can enter the blood stream through procedures that cause break in the integrity of skin like surgery, catheterisation or during access of long term indwelling catheters or secondary to intravenous injection of recreational drugs.
Enterococcus can enter the bloodstream as a consequence of abnormalities in the gastrointestinal or genitourinary tracts.
Some organisms, when isolated, give valuable clues to the cause, as they tend to be specific.
Multiple case reports of infective endocarditis caused by unusual organisms have been published. Few examples include: Propionibacterium sp., which are normal skin flora, have been responsible for infective endocarditis sometimes leading to deaths due to the indolent course of this abscess producing infection.Tropheryma whipplei has caused endocarditis without gastrointestinal involvement. Citrobacter koseri was found in an immunocompetent adult. Neisseria bacilliformis was found in a patient with a bicuspid aortic valve.
Fungal
Candida albicans, a yeast, is associated with endocarditis in IV drug users and immunocompromised patients. Other fungi demonstrated to cause endocarditis are Histoplasma capsulatum and Aspergillus. Endocarditis with Tricosporon asahii has also been reported in a case report.
Risk factors
Risk factors for infective endocarditis are based off the premise that in a healthy individual, bacteremia (bacteria entering the blood stream) is cleared quickly with no adverse consequences. However, if a heart valve is damaged, the bacteria can attach themselves to the valve, resulting in infective endocarditis. Additionally, in individuals with weakened immune systems, the concentration of bacteria in the blood can reach levels high enough to increase the probability that some will attach to the valve. Some significant risk factors are listed here:
- Artificial heart valves
- Intracardiac devices, such as Implantable cardioverter-defibrillators
- Unrepaired cyanotic congenital heart defects
- History of infective endocarditis
- Chronic rheumatic heart disease, which is an autoimmune response to repeated Streptococcus pyogenes infection
- Age-related degenerative valvular lesions
- Hemodialysis, a medical procedure that filters the blood of individuals with kidney failure
- Coexisting conditions, especially ones that suppress immunity. Diabetes mellitus, alcohol abuse, HIV/AIDS, and intravenous drug use all fall in this category
More detailed descriptions of these and other risk factors are provided below.
Other conditions that result in high number of bacteria entering into the bloodstream include colorectal cancer (mostly Streptococcus bovis), serious urinary tract infections (mostly enterococci), and drug injection (Staphylococcus aureus). With a large number of bacteria, even a normal heart valve may become infected.
A more virulent organism (such as Staphylococcus aureus) can cause infective endocarditis by infecting even a normal heart valve.
Intravenous drug users tend to get their right-sided heart valves infected because the veins that are injected drain into the right side of the heart. In rheumatic heart disease, infection occurs on the aortic and the mitral valves on the left side of the heart.
Other factors that increase the risk of developing infective endocarditis are low levels of white blood cells, immunodeficiency or immunosuppression, malignancy, diabetes mellitus, and alcohol abuse.
Dental operations
In the past, bacteremia caused by dental procedures (in most cases due to streptococci viridans, which reside in oral cavity), such as a cleaning or extraction of a tooth was thought to be more clinically significant than it actually was. However, it is important that a dentist or a dental hygienist be told of any heart problems before commencing treatment. Antibiotics are administered to patients with certain heart conditions as a precaution, although this practice has changed in the US, with new American Heart Association guidelines released in 2007, and in the UK as of March 2008 due to new NICE guidelines. Everyday tooth brushing and flossing will similarly cause bacteremia. Although there is little evidence to support antibiotic prophylaxis for dental treatment, the current American Heart Association guidelines are highly accepted by clinicians and patients.
Pathogenesis
Damaged valves and endocardium contribute to the development of infective endocarditis. Specifically, the damaged part of a heart valve forms a local blood clot, a condition known as non-bacterial thrombotic endocarditis (NBTE). The platelet and fibrin deposits that form as part of the blood clotting process allow bacteria to take hold and form vegetations. As previously mentioned, the body has no direct methods of combating valvular vegetations because the valves do not have a dedicated blood supply. This combination of damaged valves, bacterial growth, and lack of a strong immune response results in infective endocarditis.
Damage to the valves and endocardium can be caused by:
The risk factors for infective endocarditis provide a more extensive list of conditions that can damage the heart.
Diagnosis
In general, the Duke criteria should be fulfilled in order to establish the diagnosis of endocarditis. The blood tests C reactive protein (CRP) and procalcitonin have not been found to be particularly useful in helping make or rule out the diagnosis.
As the Duke criteria rely heavily on the results of echocardiography, research has addressed when to order an echocardiogram by using signs and symptoms to predict occult endocarditis among patients with intravenous drug abuse and among non drug-abusing patients. Unfortunately, this research is over 20 years old and it is possible that changes in the epidemiology of endocarditis and bacteria such as staphylococci make the following estimates incorrect.
Echocardiography
The transthoracic echocardiogram has a sensitivity and specificity of approximately 65% and 95% if the echocardiographer believes there is 'probable' or 'almost certain' evidence of endocarditis.
Modified Duke criteria
Established in 1994 by the Duke Endocarditis Service and revised in 2000, the Duke criteria are a collection of major and minor criteria used to establish a diagnosis of infective endocarditis. According to the Duke criteria, diagnosis of infective endocarditis can be definite, possible, or rejected. A diagnosis of infective endocarditis is definite if either the following pathological or clinical criteria are met:
- One of these pathological criteria:
- Histology or culture of a cardiac vegetation, an embolized vegetation, or intracardiac abscess from the heart finds microorganisms
- Active endocarditis
- One of these combinations of clinical criteria
- 2 major clinical criteria
- 1 major and 3 minor criteria
- 5 minor criteria
Diagnosis of infective endocarditis is possible if one of the following combinations of clinical criteria are met:
Major criteria
- Positive blood culture with typical IE microorganism, defined as one of the following:
- Typical microorganism consistent with IE from 2 separate blood cultures, as noted below:
- Viridans-group streptococci, or
- Streptococcus bovis including nutritional variant strains, or
- HACEK group, or
- Staphylococcus aureus, or
- Community-acquired Enterococci, in the absence of a primary focus
- Microorganisms consistent with IE from persistently positive blood cultures defined as:
- Two positive cultures of blood samples drawn >12 hours apart, or
- All of 3 or a majority of 4 separate cultures of blood (with first and last sample drawn 1 hour apart)
- Coxiella burnetii detected by at least one positive blood culture or IgG antibody titer for Q fever phase 1 antigen >1:800. This was previously a minor criterion
- Evidence of endocardial involvement with positive echocardiogram defined as
- Oscillating intracardiac mass on valve or supporting structures, in the path of regurgitant jets, or on implanted material in the absence of an alternative anatomic explanation, or
- Abscess, or
- New partial dehiscence of prosthetic valve or new valvular regurgitation (worsening or changing of preexisting murmur not sufficient)
Minor criteria
- Predisposing factor: known cardiac lesion, recreational drug injection
- Fever >38 °C
- Embolism evidence: arterial emboli, pulmonary infarcts, Janeway lesions, conjunctival hemorrhage
- Immunological problems: glomerulonephritis, Osler's nodes, Roth's spots, Rheumatoid factor
- Microbiologic evidence: Positive blood culture (that doesn't meet a major criterion) or serologic evidence of infection with organism consistent with IE but not satisfying major criterion
Positive echocardiogram (that doesn't meet a major criterion)(this criterion has been removed from the modified Duke criteria)
Risk
Among people who do not use intravenous drugs and have a fever in the emergency room, there is a less than 5% chance of occult endocarditis. Mellors in 1987 found no cases of endocarditis nor of staphylococcal bacteremia among 135 febrile patients in the emergency room. The upper confidence interval for 0% of 135 is 5%, so for statistical reasons alone, there is up to a 5% chance of endocarditis among these patients. In contrast, Leibovici found that among 113 non-selected adults admitted to the hospital because of fever there were two cases (1.8% with 95%CI: 0% to 7%) of endocarditis.
Among people who do use intravenous drugs and have a fever in the emergency room, there is about a 10% to 15% prevalence of endocarditis. This estimate is not substantially changed by whether the doctor believes the patient has a trivial explanation for their fever. Weisse found that 13% of 121 patients had endocarditis. Marantz also found a prevalence of endocarditis of 13% among such patients in the emergency room with fever. Samet found a 6% incidence among 283 such patients, but after excluding patients with initially apparent major illness to explain the fever (including 11 cases of manifest endocarditis), there was a 7% prevalence of endocarditis.
Among people with staphylococcal bacteremia (SAB), one study found a 29% prevalence of endocarditis in community-acquired SAB versus 5% in nosocomial SAB. However, only 2% of strains were resistant to methicillin and so these numbers may be low in areas of higher resistance.
Prevention
Not all people with heart disease require antibiotics to prevent infective endocarditis. Heart diseases have been classified into high, medium and low risk of developing IE. Those falling into high risk category require IE prophylaxis before endoscopies and urinary tract procedures. Diseases listed under high risk include
- Prior Endocarditis
- Unrepaired cyanotic congenital heart diseases
- Completely repaired congenital heart disease in their first 6 months
- Prosthetic heart valves
- Incompletely repaired congenital heart diseases
- Cardiac transplant valvulopathy
Following are the antibiotic regimens recommended by the American Heart Association for antibiotic prophylaxis:
Oral Amoxicillin 1 hour before the procedureIntravenous or intramuscular ampicillin 1 hour before the procedureIn patients allergic to penicillinsIn the UK, NICE clinical guidelines no longer advise prophylaxis because there is no clinical evidence that it reduces the incidence of IE and there are negative effects (e.g. allergy and increased bacterial resistance) of taking antibiotics that may outweigh the benefits.
Antibiotics were historically commonly recommended to prevent IE in those with heart problems undergoing dental procedures (known as dental antibiotic prophylaxis). They are less commonly recommended for this procedure.
Treatment
High dose antibiotics are administered by the intravenous route to maximize diffusion of antibiotic molecules into vegetation(s) from the blood filling the chambers of the heart. This is necessary because neither the heart valves nor the vegetations adherent to them are supplied by blood vessels. Antibiotics are typically continued for two to six weeks depending on the characteristics of the infection and the causative microorganisms.
In acute endocarditis, due to the fulminant inflammation empirical antibiotic therapy is started immediately after the blood has been drawn for culture. This usually includes vancomycin and ceftriaxone IV infusions until the microbial identification and susceptibility report with the minimum inhibitory concentration becomes available allowing for modification of the antimicrobial therapy to target the specific microorganism. It should be noted that the routine use of gentamicin to treat endocarditis has fallen out of favor due to the lack of evidence to support its use (except in infections caused by Enterococcus and nutritionally variant streptococci) and the high rate of complications.
In subacute endocarditis, where patient's hemodynamic status is usually stable, antibiotic treatment can be delayed till the causative microorganism can be identified.
The most common organism responsible for infective endocarditis is Staphylococcus aureus, which is resistant to penicillin in most cases. High rates of resistance to oxacillin are also seen, in which cases treatment with vancomycin is required.
Viridans group streptococci and Streptococcus bovis are usually highly susceptible to penicillin and can be treated with penicillin or ceftriaxone.
Relatively resistant strains of viridans group streptococci and Streptococcus bovis are treated with penicillin or ceftriaxone along with a shorter 2 week course of an aminoglycoside during the initial phase of treatment.
Highly penicillin resistant strains of viridans group streptococci, nutritionally variant streptococci like Granulicatella sp., Gemella sp. and Abiotrophia defectiva, and Enterococci are usually treated with a combination therapy consisting of penicillin and an aminoglycoside for the entire duration of 4–6 weeks.
Selected patients may be treated with a relatively shorter course of treatment (2 weeks) with benzyl penicillin IV if infection is caused by viridans group streptococci or Streptococcus bovis as long as the following conditions are met:
Additionally oxacillin susceptible Staphylococcus aureus native valve endocarditis of the right side can also be treated with a short 2 week course of beta lactam antibiotic like nafcillin with or without aminoglycosides
Surgical debridement of infected material and replacement of the valve with a mechanical or bioprosthetic artificial heart valve is necessary in certain situations:
‣ Patients with significant valve stenosis or regurgitation causing heart failure ‣ Evidence of hemodynamic compromise in the form of elevated end diastolic left ventricular or left atrial pressure or moderate to severe pulmonary hypertension ‣ Presence of intracardiac complications like paravalvular abscess, conduction defects or destructive penetrating lesions ‣ Recurrent septic emboli despite appropriate antibiotic treatment ‣ Large vegetations (> 10 mm) ‣ Persistent positive blood cultures despite appropriate antibiotic treatment ‣ Prosthetic valve dehiscence ‣ Relapsing infection in the presence of a prosthetic valve ‣ Abscess formation ‣ Early closure of mitral valve ‣ Infection caused by Fungi or resistant Gram negative bacteria. The guidelines were recently updated by both the American college of cardiology and the European society of cardiology. There was a recent meta analysis published that showed surgical intervention at 7 days or less is associated with lower mortality in a long term. (Reference pub med id 26869640).
Infective endocarditis is associated with 18% in-hospital mortality.
Epidemiology
In developed countries, the annual incidence of infective endocarditis is 3 to 9 cases per 100,000 persons. The male to female case ratio is over 2:1. There is an increased incidence of infective endocarditis in persons 65 years of age and older, which is probably because people in this age group have a larger number of risk factors for infective endocarditis. In recent years, over one third of infective endocarditis cases in the United States were healthcare-associated. Another trend observed in developed countries is that chronic rheumatic heart disease accounts for <10% of cases. Although a history of valve disease has a significant association with infective endocarditis, 50% of all cases develop in people with no known history of valvular disease.
