Heart murmurs are heart sounds produced when blood flows across one of the heart valves that are loud enough to be heard with a stethoscope.
There are two types of murmurs. A functional murmur or "physiologic murmur" is a heart murmur that is primarily due to physiologic conditions outside the heart. Other types of murmurs are due to structural defects in the heart itself. Functional murmurs are benign (an "innocent murmur").
Murmurs may also be the result of various problems, such as narrowing or leaking of valves, or the presence of abnormal passages through which blood flows in or near the heart. Such murmurs, known as pathologic murmurs, should be evaluated by an expert.
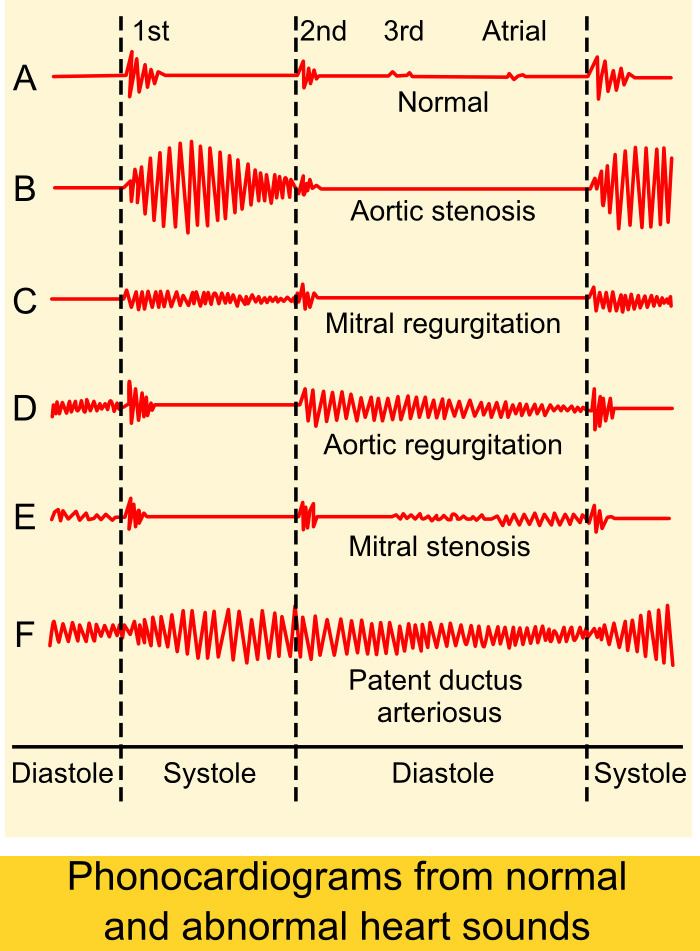
Heart murmurs are most frequently categorized by timing, into systolic heart murmurs and diastolic heart murmurs, differing in the part of the heartbeat on which they can be heard. However, continuous murmurs cannot be directly placed into either category.
Murmurs can be classified by seven different characteristics: timing, shape, location, radiation, intensity, pitch and quality.
Timing refers to whether the murmur is a systolic or diastolic murmur.Shape refers to the intensity over time; murmurs can be crescendo, decrescendo or crescendo-decrescendo. Crescendo murmurs progressively increase in intensity. Decrescendo murmurs progressively decrease in intensity. With crescendo—decrescendo murmurs (diamond or kite-shaped murmurs), a progressive increase in intensity is followed by a progressive decrease in intensity.Location refers to where the heart murmur is usually heard best. There are four places on the anterior chest wall to listen for heart murmurs; each of the locations roughly corresponds to a specific part of the heart and should be listened to (through the stethoscope) with the patient lying down, face up. The four locations are:Aortic region - the 2nd right intercostal space.Pulmonic region - the 2nd left intercostal spaces.Tricuspid region - the 4th left intercostal space.Mitral region - the 5th left mid-clavicular intercostal space.Additional maneuvers can be performed for additional
auscultation:
Left lateral decubitus.With the patient sitting upright.With the patient leaning forward and exhaling.Radiation refers to where the sound of the murmur radiates. The rule of thumb is that the sound radiates in the direction of the blood flow.Intensity refers to the loudness of the murmur, and is graded according to the Levine scale, from 1 to 6:- The murmur is only audible on listening carefully for some time.
- The murmur is faint but immediately audible on placing the stethoscope on the chest.
- A loud murmur readily audible but with no palpable thrill.
- A loud murmur with a palpable thrill.
- A loud murmur with a palpable thrill. The murmur is so loud that it is audible with only the rim of the stethoscope touching the chest.
- A loud murmur with a palpable thrill. The murmur is audible with the stethoscope not touching the chest but lifted just off it.
Pitch may be low, medium or high and is determined by whether it can be auscultated best with the bell or diaphragm of a stethoscope.Quality refers to unusual characteristics of a murmur, such as blowing, harsh, rumbling or musical.A mnemonic to remember what characteristics to look for when listening to murmurs is SCRIPT: Site, Configuration (shape), Radiation, Intensity, Pitch and quality, and Timing in the cardiac cycle.
The use of two simple mnemonics may help differentiate systolic and diastolic murmurs; PASS and PAID. Pulmonary and aortic stenoses are systolic while pulmonary and aortic insufficiency (regurgitation) are diastolic. Mitral and tricuspid defects are opposite.
Inhalation leads to an increase in intrathoracic negative pressure, which increases the capacity of pulmonary circulation, thereby prolonging ejection time. This will affect the closure of the pulmonary valve. This finding, also called Carvallo's maneuver, has been found by studies to have a sensitivity of 100% and a specificity of 80% to 88% in detecting murmurs originating in the right heart. specifically positive Carvallo's sign describes the increase in intensity of a tricuspid regurgitation murmur with inspiration.Abrupt standingSquatting, by increasing afterload and increasing preload.Handgrip maneuver, by increasing afterloadValsalva maneuver. One study found the Valsalva maneuver to have a sensitivity of 65%, specificity of 96% in detecting hypertrophic obstructive cardiomyopathy (HOCM). Both standing and Valsalva maneuver will decrease venous return and subsequently decrease left ventricular filling, resulting in an increase in the loudness of the murmur of hypertrophic cardiomyopathy, since outflow obstruction is increased by decreasing preload. Alternatively, squatting increases systemic vascular resistance, increasing afterload and helping to hold the obstruction in a more open configuration, decreasing the murmur. Maximum handgrip exercise also results in a decrease in the loudness of the murmur.Post ectopic potentiationInhaled amyl nitrite is a vasodilator that diminishes systolic murmurs in left-to-right shunts in ventricular septal defects, and reveals right-to left shunts in the setting of a pulmonic stenosis and a ventricular septal defect.MethoxaminePositioning of the patient. That is, putting patients in the left lateral position will allow a murmur in the mitral valve area to be more pronounced.Types and disease associations
Continuous machinery murmur, at the left upper sternal borderClassic for a
patent ductus arteriosus, and in serious cases associated with poor feeding, failure to thrive and respiratory distress. Other examination findings may include widened pulse pressures and bounding pulses.
Systolic murmur loudest below the left scapulaClassic for a coarctation of the aorta which is often seen in Turner's Syndrome, (
gonadal dysgenesis), an X-linked disorder with a part missing of the X-chromosome. Other findings of this murmur is radio-femoral delay, and different blood pressures in the upper and lower extremities.
Harsh holosystolic murmur at the left lower sternal borderClassic for a ventricular septal defect. It is in these children that the delayed-onset cyanotic heart disease occurs known as Eisenmenger syndrome, which is a reversal of the left-to-right heart shunt as the right ventricle hypertrophies, causing a right-to-left shunt and resulting cyanosis.
Widely split fixed S2 and systolic ejection murmur at the left upper sternal borderClassically due to a patent
foramen ovale or
atrial septal defect, which is lack of closure of the foramen ovale. This produces a left-to-right shunt initially, thus does not produce cyanosis, but causes
pulmonary hypertension. Longstanding uncorrected atrial septal defects can also result in Eisenmenger's syndrome with resultant cyanosis.
The cooing dove murmur is a cardiac murmur with a musical quality (high pitched - hence the name) and is associated with aortic valve regurgitation (or mitral regurgitation before rupture of chordae). It is a diastolic murmur which can be heard over the mid-precordium.[1]