ICD-9-CM 155 MedlinePlus 000280 | ICD-10 C22.0 ICD-O M8170/3 eMedicine med/787 | |
 | ||
Hepatocellular carcinoma (HCC), also called malignant hepatoma, is the most common type of liver cancer.
Contents
- Signs and symptoms
- Risk factors
- Pathogenesis
- Diagnosis
- Screening
- Higher risk people
- Imaging
- Pathology
- Staging
- Prevention
- Management
- Interventional radiology
- Complications
- Other treatments
- Prognosis
- Epidemiology
- Africa and Asia
- North America and Western Europe
- Pre clinical
- Clinical
- Abbreviations
- References
Most cases of HCC are as a result of either a viral hepatitis infection (hepatitis B or C), metabolic toxins such as alcohol or aflatoxin, conditions like hemochromatosis and alpha 1-antitrypsin deficiency or NASH.
Treatment options for HCC and prognosis are dependent on many factors but especially on tumor size, staging, and extent of liver injury. Tumor grade is also important; high-grade tumors will have a poor prognosis, while low-grade tumors may go unnoticed for many years, as is the case in many other organs.
HCC is relatively uncommon in the United States and many other developed countries. It occurs most commonly in countries where hepatitis B infections are common.
Signs and symptoms
Most cases of hepatocellular carcinoma occur in people who already have symptoms of chronic liver disease and present either with worsening of symptoms or during surveillance that is used to screen patients who are at risk the most. In other cases, HCC may directly present with yellow skin, bloating from fluid in the abdomen, easy bruising from blood clotting abnormalities, loss of appetite, unintentional weight loss, abdominal pain especially in the right upper quadrant, nausea, vomiting, or feeling tired.
Risk factors
The main risk factors for hepatocellular carcinoma are;
The most important risk factors vary widely from country to country. In countries where hepatitis B is endemic, such as China, hepatitis B is the predominant cause of Hepatocellular Carcinoma. Whereas in countries, such as the United States, where Hepatitis B is rare because of high vaccination rates, the major cause of HCC is Cirrhosis (often due to hepatitis C, obesity or alcohol abuse).
The risk of hepatocellular carcinoma in type 2 diabetics is greater (from 2.5 to 7.1 times the non diabetic risk) depending on the duration of diabetes and treatment protocol. A suspected contributor to this increased risk is circulating insulin concentration such that diabetics with poor insulin control or on treatments that elevate their insulin output (both states that contribute to a higher circulating insulin concentration) show far greater risk of hepatocellular carcinoma than diabetics on treatments that reduce circulating insulin concentration. On this note, some diabetics who engage in tight insulin control (by keeping it from being elevated) show risk levels low enough to be indistinguishable from the general population. This phenomenon is thus not isolated to diabetes mellitus type 2 since poor insulin regulation is also found in other conditions such as metabolic syndrome (specifically, when evidence of non alcoholic fatty liver disease or NAFLD is present) and again there is evidence of greater risk here too. While there are claims that anabolic steroid abusers are at greater risk (theorized to be due to insulin and IGF exacerbation), the only evidence that has been confirmed is that anabolic steroid users are more likely to have hepatocellular adenomas (a benign form of HCC) transform into the more dangerous hepatocellular carcinoma.
When hepatocellular adenomas grow to a size of more than 6–8 cm, they are considered cancerous and thus become a risk of hepatocellular carcinoma. Although hepatocellular carcinoma most commonly affects adults, children who are affected with biliary atresia, infantile cholestasis, glycogen-storage diseases, and other cirrhotic diseases of the liver are predisposed to developing hepatocellular carcinoma.
Children and adolescents are unlikely to have chronic liver disease, however, if they suffer from congenital liver disorders, this fact increases the chance of developing hepatocellular carcinoma.
Young adults afflicted by the rare fibrolamellar variant of hepatocellular carcinoma may have none of the typical risk factors, i.e. cirrhosis and hepatitis.
Pathogenesis
Hepatocellular carcinoma, like any other cancer, develops when there is a mutation to the cellular machinery that causes the cell to replicate at a higher rate and/or results in the cell avoiding apoptosis. In particular, chronic infections of hepatitis B and/or C can aid the development of hepatocellular carcinoma by repeatedly causing the body's own immune system to attack the liver cells, some of which are infected by the virus, others merely bystanders. While this constant cycle of damage followed by repair can lead to mistakes during repair which in turn lead to carcinogenesis, this hypothesis is more applicable, at present, to hepatitis C. Chronic hepatitis C causes HCC through the stage of cirrhosis. In chronic hepatitis B, however, the integration of the viral genome into infected cells can directly induce a non-cirrhotic liver to develop HCC. Alternatively, repeated consumption of large amounts of ethanol can have a similar effect. The toxin aflatoxin from certain Aspergillus species of fungus is a carcinogen and aids carcinogenesis of hepatocellular cancer by building up in the liver. The combined high prevalence of rates of aflatoxin and hepatitis B in settings like China and West Africa has led to relatively high rates of hepatocellular carcinoma in these regions. Other viral hepatitides such as hepatitis A have no potential to become a chronic infection and thus are not related to hepatocellular carcinoma.
Diagnosis
Methods of diagnosis in HCC have evolved with the improvement in medical imaging. The evaluation of both asymptomatic patients and those with symptoms of liver disease involves blood testing and imaging evaluation. Although historically a biopsy of the tumor was required to prove the diagnosis, imaging (especially MRI) findings may be conclusive enough to obviate histopatholgic confirmation.
Screening
Due to the fact that HCC most commonly occurs in the setting of chronic liver disease (e.g. viral hepatitis) and cirrhosis (about 80%), screening by ultrasound (US) is commonly advocated in this population. Surveillance recommendations vary, but the American Association of Liver Diseases recommends screening Asian men over the age of 40, Asian women over the age of 50, people with HBV and cirrhosis, and African and North American blacks. These people are screened with ultrasound every 6 months. Additional evaluation may include measurement of blood levels of AFP, which is a tumor marker. Elevated levels of AFP are associated with active HCC disease. At levels less >20 sensitivity is 41-65% and specificity is 80-94%. However, at levels >200 sensitivity is 31, specificity is 99%.
Ultrasound (US) is often the first imaging and screening modality used. On US, HCC often appears as a small hypoechoic lesion with poorly defined margins and coarse irregular internal echoes. When the tumor grows, it can sometimes appear heterogeneous with fibrosis, fatty change, and calcifications. This heterogeneity can look similar to cirrhosis and the surrounding liver parenchyma. A systematic review found that the sensitivity was 60 percent (95% CI 44-76%) and specificity was 97 percent (95% CI 95-98%) compared with pathologic examination of an explanted or resected liver as the reference standard. The sensitivity increases to 79% with AFP correlation.
Higher risk people
In a person where there is higher suspicion of HCC, such as a person with symptoms or abnormal blood tests (i.e. alpha-fetoprotein and des-gamma carboxyprothrombin levels), evaluation requires imaging of the liver by CT or MRI scans. Optimally, these scans are performed with intravenous contrast in multiple phases of hepatic perfusion in order to improve detection and accurate classification of any liver lesions by the interpreting radiologist. Due to the characteristic blood flow pattern of HCC tumors, a specific perfusion pattern of any detected liver lesion may conclusively detect an HCC tumor. Alternatively, the scan may detect and indeterminate lesion and further evaluation may be performed by obtaining a physical sample of the lesion.
Imaging
Ultrasound, CT scan, and MRI may be used to evaluate the liver for HCC. On CT and MRI, HCC can have three distinct patterns of growth:
A systemic review of CT diagnosis found that the sensitivity was 68 percent (95% CI 55-80%) and specificity was 93 percent (95% CI 89-96%) compared with pathologic examination of an explanted or resected liver as the reference standard. With triple-phase helical CT, the sensitivity 90% or higher, but this data has not been confirmed with autopsy studies.
However, MRI has the advantage of delivering high-resolution images of the liver without ionizing radiation. HCC appears as a high-intensity pattern on T2 weighted images and a low-intensity pattern on T1 weighted images. The advantage of MRI is that is has improved sensitivity and specificity when compared to US and CT in cirrhotic patients with whom it can be difficult to differentiate HCC from regenerative nodules. A systematic review found that the sensitivity was 81 percent (95% CI 70-91%) and specificity was 85 percent (95% CI 77-93%) compared with pathologic examination of an explanted or resected liver as the reference standard. The sensitivity is further increased if gadolinium contrast-enhanced and diffusion-weighted imaging are combined.
MRI is more sensitive and specific than CT.
Liver Image Reporting and Data System (LI-RADS) is a classification system for the reporting of liver lesions detected on CT and MRI. Radiologists use this standardized system to report on suspicious lesions and to provide an estimated likelihood of malignancy. Categories range from LI-RADS (LR) 1 to 5, in order of concern for cancer. A biopsy is not needed to confirm the diagnosis of HCC if certain imaging criteria are met.
Pathology
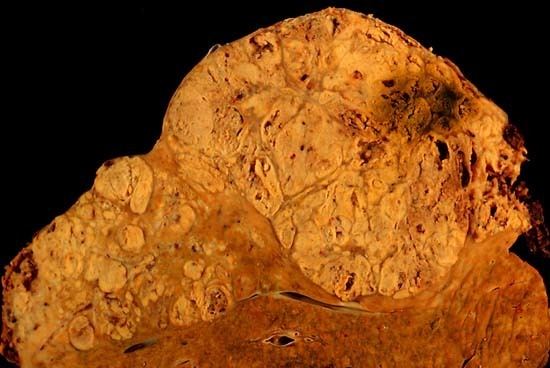
Macroscopically, liver cancer appears as a nodular or infiltrative tumor. The nodular type may be solitary (large mass) or multiple (when developed as a complication of cirrhosis). Tumor nodules are round to oval, gray or green (if the tumor produces bile), well circumscribed but not encapsulated. The diffuse type is poorly circumscribed and infiltrates the portal veins, or the hepatic veins (rarely).
Microscopically, there are four architectural and cytological types (patterns) of hepatocellular carcinoma: fibrolamellar, pseudoglandular (adenoid), pleomorphic (giant cell) and clear cell. In well-differentiated forms, tumor cells resemble hepatocytes, form trabeculae, cords, and nests, and may contain bile pigment in the cytoplasm. In poorly differentiated forms, malignant epithelial cells are discohesive, pleomorphic, anaplastic, giant. The tumor has a scant stroma and central necrosis because of the poor vascularization.
Staging
The prognosis of HCC is affected by the staging of the tumour as well as the livers function due to the effects of liver cirrhosis.
There are a number of staging classifications for HCC available however due to the unique nature of the carcinoma in order to fully encompass all the features that affect the categorization of the HCC, a classification system should incorporate; tumor size and number, presence of vascular invasion and extrahepatic spread, liver function (levels of serum bilirubin and albumin, presence of ascites and portal hypertension) and general health status of the patient (defined by the ECOG classification and the presence of symptoms).
Out of all the staging classification systems available the Barcelona Clinic Liver Cancer (BCLC) staging classification encompasses all of the above characteristics. This staging classification can be used in order to select people for treatment.
Important features that guide treatment include: -
MRI is the best imaging method to detect the presence of a tumor capsule.
Prevention
Since hepatitis B or C is one of the main causes of hepatocellular carcinoma, prevention of this infection is key to then prevent hepatocellular carcinoma. Thus, childhood vaccination against hepatitis B may reduce the risk of liver cancer in the future.
In the case of patients with cirrhosis, alcohol consumption is to be avoided. Also, screening for hemochromatosis may be beneficial for some patients.
It is unclear if screening those with chronic liver disease for hepatocellular carcinoma improves outcomes.
Management
Interventional radiology
Complications
The most common complication of both TACE and SIRT is post-embolization syndrome occurring in 60-80% of patients in TACE and 20-55% in SIRT. Typical findings of post-embolization syndrome are fatigue, constitutional symptoms and abdominal pain. It usually lasts 3–4 days with full resolution in 7–10 days. Other more serious complications from TACE and SIRT include liver failure, hepatic dysfunction and gastric ulceration from non-target embolization of the left gastric. Less than 1% of patients who undergo SIRT develop radiation pneumonitis. Complications of RFA are rare but include abscess formation, subcapsular hematoma, and tract seeding.
While surgical resection offers the best chance at a cure for hepatocellular carcinoma, the tumors are often inoperable due to the large size or spread into vascular and adjacent structures. Medical management is generally palliative and aimed at reducing liver disease symptoms. Chemotherapy is traditionally ineffective. Interventional radiology offers minimally invasive treatments that can improve quality of life, increase survival, and reduce symptoms in these patients.
Other treatments
Prognosis
The usual outcome is poor, because only 10–20% of hepatocellular carcinomas can be removed completely using surgery. If the cancer cannot be completely removed, the disease is usually deadly within 3 to 6 months. This is partially due to late presentation with tumors, but also the lack of medical expertise and facilities in the regions with high HCC prevalence. However, survival can vary, and occasionally people will survive much longer than 6 months. The prognosis for metastatic or unresectable hepatocellular carcinoma has recently improved due to the approval of sorafenib (Nexavar®) for advanced hepatocellular carcinoma.
Epidemiology
HCC is one of the most common tumors worldwide. The epidemiology of HCC exhibits two main patterns, one in North America and Western Europe and another in non-Western countries, such as those in sub-Saharan Africa, central and Southeast Asia, and the Amazon basin. Males are affected more than females usually and it is most common between the age of 30 to 50, Hepatocellular carcinoma causes 662,000 deaths worldwide per year about half of them in China.
Africa and Asia
In some parts of the world, such as sub-Saharan Africa and Southeast Asia, HCC is the most common cancer, generally affecting men more than women, and with an age of onset between late teens and 30s. This variability is in part due to the different patterns of hepatitis B and hepatitis C transmission in different populations - infection at or around birth predispose to earlier cancers than if people are infected later. The time between hepatitis B infection and development into HCC can be years, even decades, but from diagnosis of HCC to death the average survival period is only 5.9 months according to one Chinese study during the 1970-80s, or 3 months (median survival time) in Sub-Saharan Africa according to Manson's textbook of tropical diseases. HCC is one of the deadliest cancers in China where chronic hepatitis B is found in 90% of cases. In Japan, chronic hepatitis C is associated with 90% of HCC cases. Food infected with Aspergillus flavus (especially peanuts and corns stored during prolonged wet seasons) which produces aflatoxin poses another risk factor for HCC.
North America and Western Europe
Most malignant tumors of the liver discovered in Western patients are metastases (spread) from tumors elsewhere. In the West, HCC is generally seen as a rare cancer, normally of those with pre-existing liver disease. It is often detected by ultrasound screening, and so can be discovered by health-care facilities much earlier than in developing regions such as Sub-Saharan Africa.
Acute and chronic hepatic porphyrias (acute intermittent porphyria, porphyria cutanea tarda, hereditary coproporphyria, variegate porphyria) and tyrosinemia type I are risk factors for hepatocellular carcinoma. The diagnosis of an acute hepatic porphyria (AIP, HCP, VP) should be sought in patients with hepatocellular carcinoma without typical risk factors of hepatitis B or C, alcoholic liver cirrhosis or hemochromatosis. Both active and latent genetic carriers of acute hepatic porphyrias are at risk for this cancer, although latent genetic carriers have developed the cancer at a later age than those with classic symptoms. Patients with acute hepatic porphyrias should be monitored for hepatocellular carcinoma.
Pre-clinical
Current research includes the search for the genes that are disregulated in HCC, anti-heparanase antibodies, protein markers, non-coding RNAs (such as TUC338) and other predictive biomarkers. As similar research is yielding results in various other malignant diseases, it is hoped that identifying the aberrant genes and the resultant proteins could lead to the identification of pharmacological interventions for HCC.
Clinical
JX-594, an oncolytic virus, has orphan drug designation for this condition and is undergoing clinical trials.
Hepcortespenlisimut-L, an oral cancer vaccine also has US FDA orphan drug designation for hepatocellular carcinoma.
A randomized trial of people with advanced HCC showed no benefit for the combination of everolimus and pasireotide.
Abbreviations
HCC, hepatocellular carcinoma; TACE, transarterial embolization/chemoembolization; PFS, progression-free survival; PS, performance status; HBV, hepatitis B virus; PEI, percutaneous ethanol injection; RFA, radiofrequency ablation; RR, response rate; MS, median survival.
