Specialty Infectious disease ICD-9-CM 003.0 MedlinePlus 000294 | ICD-10 A02.0 DiseasesDB 11765 | |
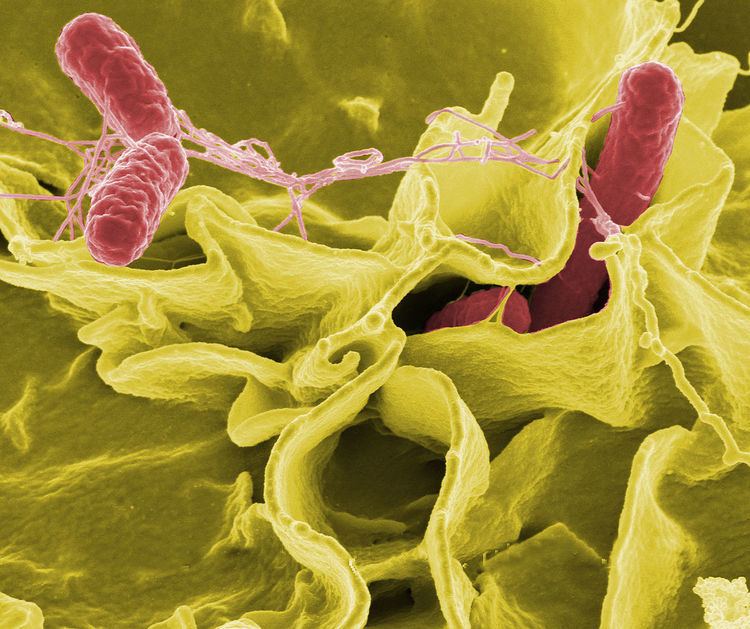 | ||
Salmonellosis is an infection caused by the Salmonella bacteria. Most people with salmonellosis develop diarrhea, fever, vomiting, and abdominal cramps 12 to 72 hours after infection. In most cases, the illness lasts four to seven days, and most people recover without treatment. In some cases, the diarrhea may be so severe that the patient becomes dangerously dehydrated and must be hospitalized.
Contents
- Enteritis
- Typhoid fever
- Long term
- Causes
- Prevention
- Vaccine
- Industrial hygiene
- Treatment
- Epidemiology
- United States
- Europe
- Elsewhere
- History
- Four inch regulation
- References
Intravenous fluids may be used to treat dehydration. Medications may be used to provide symptomatic relief, such as fever reduction. In severe cases, the Salmonella infection may spread from the intestines to the blood stream, and then to other body sites; this is known as typhoid fever and is treated with antibiotics.
The elderly, infants, and those with impaired immune systems are more likely to develop severe illness. Some people afflicted with salmonellosis later experience reactive arthritis, which can have long-lasting, disabling effects. The only two species of Salmonella are Salmonella bongori and Salmonella enterica. The latter is divided in six subspecies: S. e. enterica, S. e. salamae, S. e. arizonae, S. e. diazonae, S. e. houtenase, and S. e. indica. These subspecies are further divided into numerous serovars. Because the serovars only differ in serotypes, and therefore in infection potential, the serovars are not italicised and are written with a capital letter as they still belong to the same subspecies.
The species Salmonella enterica subsp. enterica contains over 60% of the total number of serovars and 99% of the serovars that are capable of infecting cold- and warm-blooded animals, as well as humans. Infections are usually contracted from sources such as:
Reptiles such as red-eared slider turtles and green iguanas may carry Salmonella bongori (which inhabits cold-blooded animals) in their intestines, which can cause intestinal infections. The most severe human Salmonella infection is caused by S. enterica subsp. enterica ser. typhi which leads to typhoid fever, an infection that often proves fatal if not treated with the appropriate antibiotics. This serovar is restricted to humans and is usually contracted through direct contact with the fecal matter of an infected person. Typhoid fever is endemic in the developing world, where unsanitary conditions are more likely to prevail, and which can affect as many as 21.5 million people each year. Recorded cases of typhoid fever in the developed world are mostly related to recent travel in areas where Salmonella typhi is endemic.
Enteritis
After a short incubation period of a few hours to one day, the bacteria multiply in the intestinal lumen, causing an intestinal inflammation. Most people with salmonellosis develop diarrhea, fever, vomiting, and abdominal cramps 12 to 72 hours after infection. Diarrhea is often mucopurulent (containing mucus or pus) and bloody. In most cases, the illness lasts four to seven days, and most people recover without treatment. In some cases, though, the diarrhea may be so severe that the patient becomes dangerously dehydrated and must be taken to a hospital. At the hospital, the patient may receive intravenous fluids to treat the dehydration, and may be given medications to provide symptomatic relief, such as fever reduction. In severe cases, the Salmonella infection may spread from the intestines to the blood stream, and then to other body sites, and can cause death, unless the person is treated promptly with antibiotics.
In otherwise healthy adults, the symptoms can be mild. Normally, no sepsis occurs, but it can occur exceptionally as a complication in the immunocompromised. However, in people at risk such as infants, small children, and the elderly, Salmonella infections can become very serious, leading to complications. In infants, dehydration can cause a state of severe toxicity. Extraintestinal localizations are possible, especially Salmonella meningitis in children, osteitis, etc. Children with sickle-cell anemia who are infected with Salmonella may develop osteomyelitis. Treatment of osteomyelitis, in this case, will be to use fluoroquinolones (ciprofloxacin, levofloxacin, etc., and nalidixic acid).
Those whose only symptom is diarrhea usually completely recover, but their bowel habits may not return to normal for several months.
Typhoid fever
Typhoid fever occurs when Salmonella bacteria enter the lymphatic system and cause a systemic form of salmonellosis. Endotoxins first act on the vascular and nervous apparatus, resulting in increased permeability and decreased tone of the vessels, upset thermal regulation, vomiting, and diarrhea. In severe forms of the disease, enough liquid and electrolytes are lost to upset the water-salt metabolism, decrease the circulating blood volume and arterial pressure, and cause hypovolemic shock. Septic shock may also develop. Shock of mixed character (with signs of both hypovolemic and septic shock) are more common in severe salmonellosis. Oliguria and azotemia develop in severe cases as a result of renal involvement due to hypoxia and toxemia.
Long-term
Salmonellosis is associated with later irritable bowel syndrome and inflammatory bowel disease. Evidence however does not support it being a direct cause of the latter.
A small number of people afflicted with salmonellosis experience reactive arthritis, which can last months or years and can lead to chronic arthritis. In sickle-cell anemia, osteomyelitis due to Salmonella infection is much more common than in the general population. Though Salmonella infection is frequently the cause of osteomyelitis in sickle-cell anemia patients, it is not the most common cause, which remains to be Staphylococcus infection.
Those infected may become asymptomatic carriers, but it is relatively uncommon, with shedding observed in only 0.2 to 0.6% of cases after a year.
Causes
Salmonella bacteria can survive for some time without a host; thus, they are frequently found in polluted water, with contamination from the excrement of carrier animals being particularly important.
The European Food Safety Authority highly recommends that when handling raw turkey meat, consumers and people involved in the food supply chain should pay attention to personal and food hygiene.
An estimated 142,000 Americans are infected each year with Salmonella Enteritidis from chicken eggs, and about 30 die. The shell of the egg may be contaminated with Salmonella by feces or environment, or its interior (yolk) may be contaminated by penetration of the bacteria through the porous shell or from a hen whose infected ovaries contaminate the egg during egg formation.
Nevertheless, such interior egg yolk contamination is theoretically unlikely. Even under natural conditions, the rate of infection was very small (0.6% in a study of naturally contaminated eggs and 3.0% among artificially and heavily infected hens).
Prevention
The FDA has published guidelines to help reduce the chance of food-borne salmonellosis. Food must be cooked to 68–72°C (145–160°F), and liquids such as soups or gravies must be boiled. Freezing kills some Salmonella, but it is not sufficient to reliably reduce them below infectious levels. While Salmonella is usually heat-sensitive, it does acquire heat resistance in high-fat environments such as peanut butter.
Vaccine
Antibodies against nontyphoidal Salmonella were first found in Malawi children in research published in 2008. The Malawian researchers have identified an antibody that protects children against bacterial infections of the blood caused by nontyphoidal Salmonella. A study at Queen Elizabeth Hospital in Blantyre found that children up to two years old develop antibodies that aid in killing the bacteria. This could lead to a possible Salmonella vaccine for humans.
A recent study has tested a vaccine on chickens which offered efficient protection against salmonellosis.
Vaccination of chickens against Salmonella essentially wiped out the disease in the United Kingdom. A similar approach has been considered in the United States, but the Food and Drug Administration decided not to mandate vaccination of hens.
Industrial hygiene
Since 2011, Denmark has had zero cases of human salmonella poisoning. The country eradicated salmonella without vaccines and antibiotics by focusing on eliminating the infection from "breeder stocks", implementing various measures to prevent infection, and taking a zero-tolerance policy towards salmonella in chickens.
Treatment
Electrolytes may be replenished with oral rehydration supplements (typically containing salts sodium chloride and potassium chloride).
Appropriate antibiotics, such as ceftriaxone, may be given to kill the bacteria but are not necessary in most cases. Azithromycin has been suggested to be better at treating typhoid in resistant populations than both fluoroquinolone drugs and ceftriaxone. Antibiotic resistance rates are increasing throughout the world, so health care providers should check current recommendations before choosing an antibiotic.
Epidemiology
In the mid- to late 20th century, Salmonella enterica serovar Enteritidis was a common contaminant of eggs. Depending on the region, this is less common now with the advent of hygiene measures in egg production, and the vaccination of laying hens to prevent Salmonella colonization. Various Salmonella serovars (strains) also cause severe diseases in animals.
United States
About 142,000 people in the United States are infected each year with Salmonella Enteritidis from chicken eggs, and about 30 die.
In 2010, an analysis of death certificates in the United States identified a total of 1,316 Salmonella-related deaths from 1990 to 2006. These were predominantly among older adults and those who were immunocompromised. The U.S. government reported as many as 20% of all chickens were contaminated with Salmonella in the late 1990s, and 16.3% were contaminated in 2005.
The United States has struggled to control salmonella infections, with the rate of infection rising from 2001 to 2011. In 1998, the USDA moved to close plants if salmonella was found in excess of 20 percent, which was the industry’s average at the time, for three consecutive tests. Texas-based Supreme Beef Processors, Inc. sued on the argument that Salmonella is naturally occurring and ultimately prevailed when a federal appeals court affirmed a lower court. These issues were highlighted in a proposed Kevin's Law (formally proposed as the Meat and Poultry Pathogen Reduction and Enforcement Act of 2003), of which components were included the Food Safety Modernization Act passed in 2011, but that law applies only to the FDA and not the USDA. The USDA proposed a regulatory initiative in 2011 to Office of Management and Budget.
Europe
Since July 2012, an outbreak of salmonellosis occurred in Northern Europe caused by Salmonella thompson. The infections were linked to smoked salmon from the manufacturer Foppen, where the contamination had occurred. Most infections were reported in the Netherlands, over 1060 infections with this subspecies have been confirmed, as well as four mortalities.
A case of widespread infection was detected mid-2012 in seven EU countries. Over 400 people had been infected with Salmonella enterica serovar Stanley (S. Stanley) that usually appears in the regions of Southeast Asia. After several DNA analyses seemed to point to a specific Belgian strain, the "Joint ECDC/E FSA Rapid Risk Assessment" report detected turkey production as the source of infection.
In Germany, food poisoning infections must be reported. Between 1990 and 2005, the number of officially recorded cases decreased from about 200,000 to about 50,000 cases.
Elsewhere
In March 2007, around 150 people were diagnosed with salmonellosis after eating tainted food at a governor's reception in Krasnoyarsk, Russia. Over 1,500 people attended the ball on March 1, and fell ill as a consequence of ingesting Salmonella-tainted sandwiches.
About 150 people were sickened by Salmonella-tainted chocolate cake produced by a major bakery chain in Singapore, in December 2007.[1]
History
Both salmonellosis and the Salmonella genus of microorganisms derive their names from a modern Latin coining after Daniel E. Salmon (1850–1914), an American veterinary surgeon. He had help from Theobald Smith, and together they found the bacterium in pigs.
Four-inch regulation
The "Four-inch regulation" or "Four-inch law" is a colloquial name for a regulation issued by the U.S. FDA in 1975, restricting the sale of turtles with a carapace length less than four inches (10 cm).
The regulation was introduced, according to the FDA, "because of the public health impact of turtle-associated salmonellosis." Cases had been reported of young children placing small turtles in their mouths, which led to the size-based restriction.
