Latin insulae pancreaticae FMA 16016 76489, 16016 | TA A05.9.01.019 | |
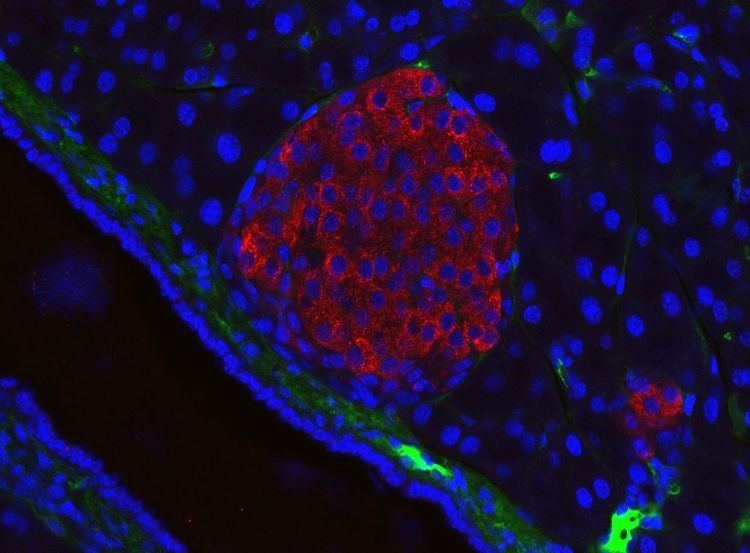 | ||
The pancreatic islets or islets of Langerhans are the regions of the pancreas that contain its endocrine (i.e., hormone-producing) cells, discovered in 1869 by German pathological anatomist Paul Langerhans. New studies show that the pancreatic islets constitute approximately 4.5% of the pancreas volume and receive 10-15% of its blood flow. The islets of Langerhans are arranged in density routes throughout the healthy human pancreas.
Contents
Structure
There are about 3 million islets distributed in the form of density routes throughout the pancreas of a healthy adult human, each of which measures an average of about 0.1 mm (109 µm) in diameter.:914 Each is separated from the surrounding pancreatic tissue by a thin fibrous connective tissue capsule which is continuous with the fibrous connective tissue that is interwoven throughout the rest of the pancreas.:914 The combined mass of the islets is 2 grams. Islets of Langerhans can also form super structures called Islet clusters which are composed of small islets that surround large blood vessels. The roundness of islets along the pancreas has also been quantified through the Index of Sphericity method. Thus, the islets closest to the spherical form are mainly found in the pancreas tail whereas the islets farthest from the spherical form are found in the pancreas neck.
Histology
Hormones produced in the pancreatic islets are secreted directly into the blood flow by (at least) five types of cells. In rat islets, endocrine cell subsets are distributed as follows:
It has been recognized that the cytoarchitecture of pancreatic islets differs between species. In particular, while rodent islets are characterized by a predominant proportion of insulin-producing beta cells in the core of the cluster and by scarce alpha, delta and PP cells in the periphery, human islets display alpha and beta cells in close relationship with each other throughout the cluster.
Islets can influence each other through paracrine and autocrine communication, and beta cells are coupled electrically to other beta cells (but not to other cell types).
Function
The paracrine feedback system of the pancreatic islets has the following structure:
A large number of G protein-coupled receptors (GPCRs) regulate the secretion of insulin, glucagon and somatostatin from pancreatic islets, and some of these GPCRs are the targets of drugs used to treat type-2 diabetes (ref GLP-1 receptor agonists, DPPIV inhibitors).b
Electrical activity
Electrical activity of pancreatic islets has been studied using patch clamp techniques. It has turned out that the behavior of cells in intact islets differs significantly from the behavior of dispersed cells.
Diabetes
The beta cells of the pancreatic islets secrete insulin, and so play a significant role in diabetes. It is thought that they are destroyed by immune assaults. However, there are also indications that beta cells have not been destroyed but have only become non-functional.
Transplantation
Because the beta cells in the pancreatic islets are selectively destroyed by an autoimmune process in type 1 diabetes, clinicians and researchers are actively pursuing islet transplantation as a means of restoring physiological beta cell function, which would offer an alternative to a complete pancreas transplant or artificial pancreas. Islet transplantation emerged as a viable option for the treatment of insulin requiring diabetes in the early 1970s with steady progress over the last three decades. Recent clinical trials have shown that insulin independence and improved metabolic control can be reproducibly obtained after transplantation of cadaveric donor islets into patients with unstable type 1 diabetes.
Islet transplantation for type 1 diabetes currently requires potent immunosuppression to prevent host rejection of donor islets.
An alternative source of beta cells, such insulin-producing cells derived from adult stem cells or progenitor cells would contribute to overcoming the shortage of donor organs for transplantation. The field of regenerative medicine is rapidly evolving and offers great hope for the nearest future. However, type 1 diabetes is the result of the autoimmune destruction of beta cells in the pancreas. Therefore, an effective cure will require a sequential, integrated approach that combines adequate and safe immune interventions with beta cell regenerative approaches.
Another potential source of beta cells may be xenotransplantation. The most likely source for xenogeneic islets for transplantation into human under evaluation is the pig pancreas. Interestingly, human and porcine insulin differ only for one amino acid, and insulin extracted from porcine pancreata has been used for the treatment of patients with diabetes before the development of recombinant human insulin technology. Several studies in small and large animals models have shown that transplantation of islet cells across species is possible. However, several problems need to be overcome for porcine islet transplantation to become a viable clinical option. The immunogenicity of xenogeneic tissues may be different from and even stronger than allogeneic tissues. For instance, Galalpha1-3Galbeta1-4GlcNAc (alpha galactosidase, alpha-Gal) expressed on porcine cells represents a major barrier to xenotransplantation being the target of preformed antibodies present in human blood.
Remarkable progress has been recorded in the development of genetically modified pigs lacking or overexpressing molecules that may improve acceptance of transplanted tissues across into humans. Pigs lacking alpha-Gal or overexpressing human decay accelerating factor (hDAF), amongst others, have been generated to study the impact on transplanted outcome in nonhuman primate models. Another possible antigenic target is the Hanganutziu-Deichter antigen, a sialic acid found in pigs and not humans, which may contribute to immunogenicity of porcine islets. Another limitation is the risk for transmission of zoonotic infections from pigs to humans, particularly from porcine endogenous retro-viruses (PERV). Amongst the approaches proposed to overcome islet xenorejection is immunoisolation of the clusters using encapsulation techniques that may shield them from immune attack. Studies in rodents and large animals have shown great promise that justify cautious optimism for the near future. Nonrandomized, uncontrolled pilot clinical trials are ongoing in subject with insulin-requiring diabetes to test the efficacy of encapsulation techniques to protect xenogeneic islets in the absence of chronic anti-rejection drugs.
