ICD-9-CM 431 | ICD-10 I61, P10.1 MeSH D002543 | |
 | ||
Synonyms cerebral haemorrhage, cerebral hemorrhage, intra-axial hemorrhage, cerebral hematoma, cerebral bleed | ||
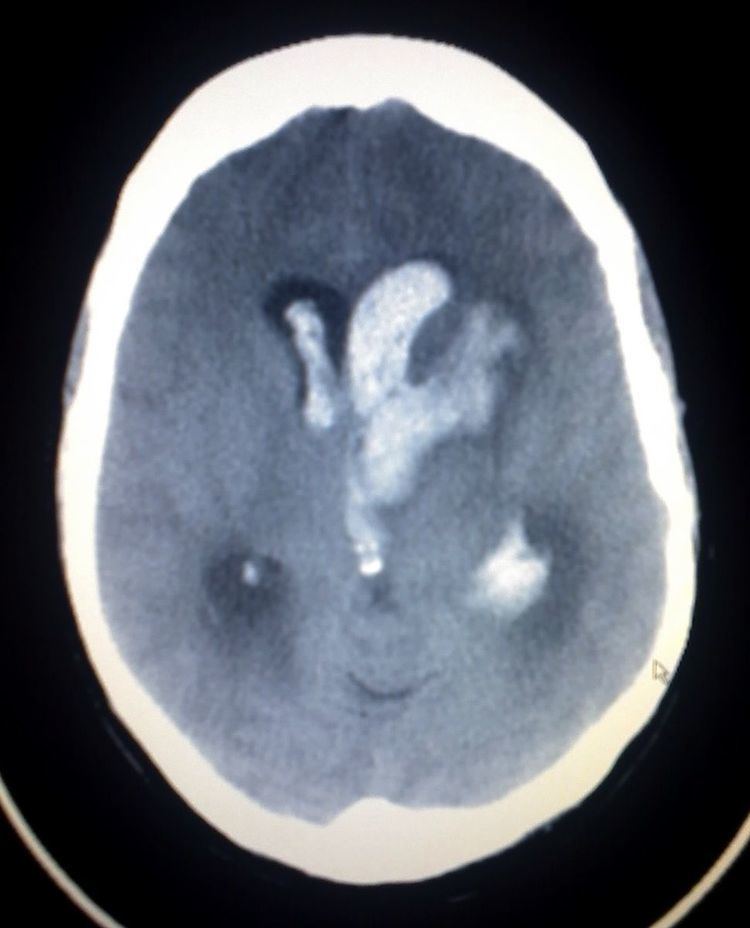
Intracerebral hemorrhage (ICH), also known as cerebral bleed, is a type of intracranial bleed that occurs within the brain tissue or ventricles. Symptoms can include headache, one-sided weakness, vomiting, seizures, decreased level of consciousness, and neck stiffness. Often symptoms get worse over time. Fever is also common. In many cases bleeding is present in both the brain tissue and the ventricles.
Contents
- Signs and symptoms
- Causes
- Diagnosis
- Location
- Treatment
- Medication
- Surgery
- Other treatment
- Prognosis
- Epidemiology
- References
Causes include brain trauma, aneurysms, arteriovenous malformations, and brain tumors. The largest risk factors for spontaneous bleeding are high blood pressure and amyloidosis. Other risk factors include alcoholism, low cholesterol, blood thinners, and cocaine. Diagnosis is typically by CT scan. Other conditions that may present similarly include ischemic stroke.
Treatment should typically be carried out in an intensive care unit. Guidelines recommended decreasing the blood pressure to a systolic of less than 140 mmHg. Blood thinners should be reversed if possible and blood sugar kept in the normal range. Surgery to place a ventricular drain may be used to treat hydrocephalus but corticosteroids should not be used. Surgery to remove the blood is useful in certain cases.
Cerebral bleeding affects about 2.5 per 10,000 people each year. It occurs more often in males and older people. About 44% of those affected die within a month. A good outcome occurs in about 20% of those affected. Strokes were first divided into their two major types, bleeding and insufficient blood flow, in 1823.
Signs and symptoms
Patients with intraparenchymal bleeds have symptoms that correspond to the functions controlled by the area of the brain that is damaged by the bleed. Other symptoms include those that indicate a rise in intracranial pressure caused by a large mass putting pressure on the brain. Intracerebral hemorrhages are often misdiagnosed as subarachnoid hemorrhages due to the similarity in symptoms and signs. A severe headache followed by vomiting is one of the more common symptoms of intracerebral hemorrhage. Another common symptom is a patient can collapse. Some people may experience continuous bleeding from the ear. Some patients may also go into a coma before the bleed is noticed.
Causes
Intracerebral bleeds are the second most common cause of stroke, accounting for 10% of hospital admissions for stroke. High blood pressure raises the risks of spontaneous intracerebral hemorrhage by two to six times. More common in adults than in children, intraparenchymal bleeds are usually due to penetrating head trauma, but can also be due to depressed skull fractures. Acceleration-deceleration trauma, rupture of an aneurysm or arteriovenous malformation (AVM), and bleeding within a tumor are additional causes. Amyloid angiopathy is a not uncommon cause of intracerebral hemorrhage in patients over the age of 55. A very small proportion is due to cerebral venous sinus thrombosis. Infection with the k serotype of Streptococcus mutans may also be a risk factor, because of its prevalence in stroke patients and production of collagen-binding protein.
Risk factors for ICH include:
Tramautic intracerebral hematomas are divided into acute and delayed. Acute intracerebral hematomas occur at the time of the injury while delayed intracerebral hematomas have been reported from as early as 6 hours post injury to as long as several weeks.
Diagnosis
Both computed tomography angiography (CTA) and magnetic resonance angiography (MRA) have been proved to be effective in diagnosing intracranial vascular malformations after ICH. So frequently, a CT angiogram will be performed in order to exclude a secondary cause of hemorrhage or to detect a "spot sign".
Intraparenchymal hemorrhage can be recognized on CT scans because blood appears brighter than other tissue and is separated from the inner table of the skull by brain tissue. The tissue surrounding a bleed is often less dense than the rest of the brain because of edema, and therefore shows up darker on the CT scan.
Location
When due to high blood pressure, they typically occur in the putamen or thalamus (60%), cerebrum (20%), cerebellum (13) or pons (7%).
Treatment
Treatment depends substantially of the type of ICH. Rapid CT scan and other diagnostic measures are used to determine proper treatment, which may include both medication and surgery.
Medication
Surgery
Surgery is required if the hematoma is greater than 3 cm (1 in), if there is a structural vascular lesion or lobar hemorrhage in a young patient.
Other treatment
Prognosis
The risk of death from an intraparenchymal bleed in traumatic brain injury is especially high when the injury occurs in the brain stem. Intraparenchymal bleeds within the medulla oblongata are almost always fatal, because they cause damage to cranial nerve X, the vagus nerve, which plays an important role in blood circulation and breathing. This kind of hemorrhage can also occur in the cortex or subcortical areas, usually in the frontal or temporal lobes when due to head injury, and sometimes in the cerebellum.
For spontaneous ICH seen on CT scan, the death rate (mortality) is 34–50% by 30 days after the insult, and half of the deaths occur in the first 2 days. Even though the majority of deaths occurs in the first days after ICH, survivors have a long term excess mortality of 27% compared to the general population.
The inflammatory response triggered by stroke has been viewed as harmful in the early stage, focusing on blood-borne leukocytes, neutrophils and macrophages, and resident microglia and astrocytes. A human postmortem study shows that inflammation occurs early and persists for several days after ICH. New area of interest are the Mast Cells.
Epidemiology
It accounts for 20% of all cases of cerebrovascular disease in the United States, behind cerebral thrombosis (40%) and cerebral embolism (30%).
It is two or more times more common in black than white people.
