Trade names Tarceva MedlinePlus a605008 Molar mass 393.436 g/mol Bioavailability 59% | AHFS/Drugs.com Monograph Routes ofadministration Oral tablets CAS ID 183321-74-6 Protein binding 95% | |
 | ||
License data EU EMA: TarcevaUS FDA: Erlotinib Pregnancycategory US: D (Evidence of risk) | ||
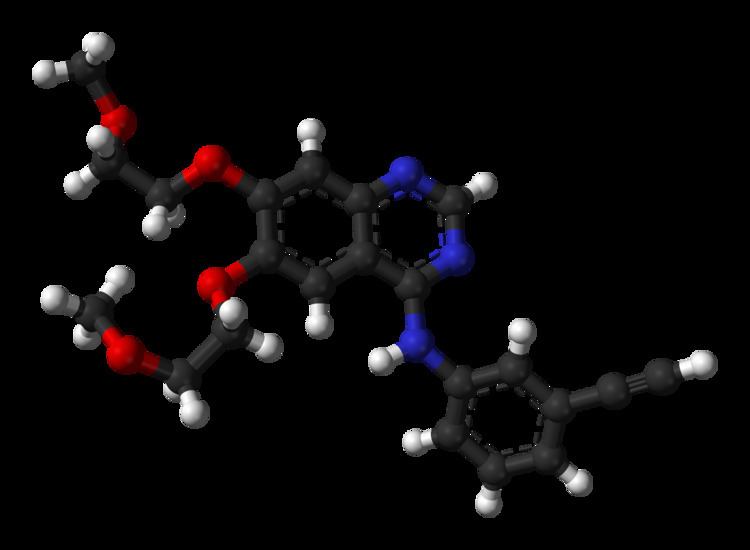
Erlotinib hydrochloride (trade name Tarceva) is a drug used to treat non-small cell lung cancer (NSCLC), pancreatic cancer and several other types of cancer. It is a receptor tyrosine kinase inhibitor, which acts on the epidermal growth factor receptor (EGFR).
Contents
It is marketed in the United States by Genentech and OSI Pharmaceuticals and elsewhere by Roche. In the United States as of 2015 one 150 mg pill costs between 200 and 242 USD.
Medical uses
Erlotinib has shown a survival benefit in the treatment of lung cancer in phase III trials. The SATURN (Sequential Tarceva in Unresectable NSCLC) study found that erlotinib added to chemotherapy improved overall survival by 19%, and improved progression-free survival (PFS) by 29%, when compared to chemotherapy alone.
The U.S. Food and Drug Administration (FDA) has approved erlotinib for the treatment of locally advanced or metastatic non-small cell lung cancer that has failed at least one prior chemotherapy regimen.
In November 2005, the FDA approved erlotinib in combination with gemcitabine for treatment of locally advanced, unresectable, or metastatic pancreatic cancer.
In lung cancer, erlotinib has been shown to be effective in patients with or without EGFR mutations, but appears to be more effective in patients with EGFR mutations. Overall survival, progression-free survival and one-year survival are similar to standard second-line therapy (docetaxel or pemetrexed). Overall response rate is about 50% better than standard second-line chemotherapy. Patients who are non-smokers, and light former smokers, with adenocarcinoma or subtypes like BAC are more likely to have EGFR mutations, but mutations can occur in all types of patients. A test for the EGFR mutation in cancer patients has been developed by Genzyme.
Erlotinib has recently been shown to be a potent inhibitor of JAK2V617F activity. JAK2V617F is a mutant of tyrosine kinase JAK2, is found in most patients with polycythemia vera (PV) and a substantial proportion of patients with idiopathic myelofibrosis or essential thrombocythemia. The study suggests that erlotinib may be used for treatment of JAK2V617F-positive PV and other myeloproliferative disorders.
The drug's US patent will expire in 2020. In May 2012, the US District Court of Delaware passed an order in favour of OSI Pharmaceutical LLC against Mylan Pharmaceuticals upholding the validity of the patent for Erlotinib. In India, generic pharmaceutical firm Cipla is battling with Roche against the Indian patent for this drug.
Common
Rare
Interactions
As per published report, erlotinib is not a substrate for either of hepatic OATPs (OATP1B1 or OATP1B3). Also, erlotinib is not an inhibitor of OATP-1B1 or OATP-1B3 transporter.
Erlotinib is mainly metabolized by the liver enzyme CYP3A4. Compounds which induce this enzyme (i.e. stimulate its production), such as St John's wort, can lower erlotinib concentrations, while inhibitors can increase concentrations.
Resistance to treatment
As with other ATP competitive small molecule tyrosine kinase inhibitors, such as imatinib (Gleevec) in CML, patients rapidly develop resistance. In the case of erlotinib this typically occurs 8–12 months from the start of treatment. Over 50% of resistance is caused by a mutation in the ATP binding pocket of the EGFR kinase domain involving substitution of a small polar threonine residue with a large nonpolar methionine residue (T790M). While proponents of the 'gatekeeper' mutation hypothesis suggest this mutation prevents the binding of erlotinib through steric hindrance, research suggests that T790M confers an increase in ATP binding affinity, thereby reducing the inhibitory efficacy of erlotinib.
Approximately 20% of drug resistance is caused by amplification of the hepatocyte growth factor receptor, which drives ERBB3 dependent activation of PI3K.
Other cases of resistance can involve numerous mutations, including recruitment of a mutated IGF-1 receptor to dimerise with EGFR so forming a heterodimer. This allows activation of the downstream effectors of EGFR even in the presence of an EGFR inhibitor. Some IGR-1R inhibitors are in various stages of development (based either around TKIs such as AG1024 or AG538 or pyrrolo[2,3-d]-pyrimidine derivatives such as NVP-AEW541). The monoclonal antibody figitumumab which targets the IGF-1R is currently undergoing clinical trials.
Another cause of resistance can be inactivating mutations of the PTEN tumour suppressor, which allow increased activation of Akt independent of stimulation by EGFR.
The most promising approach to combating resistance is likely to be combination therapy. Commencing treatment with a number of different therapeutic agents with differing modes of action is thought to provide the best defence against development of T790M and other resistance conferring mutations.
Mechanism
Erlotinib is an epidermal growth factor receptor inhibitor (EGFR inhibitor). The drug follows Iressa (gefitinib), which was the first drug of this type. Erlotinib specifically targets the epidermal growth factor receptor (EGFR) tyrosine kinase, which is highly expressed and occasionally mutated in various forms of cancer. It binds in a reversible fashion to the adenosine triphosphate (ATP) binding site of the receptor. For the signal to be transmitted, two EGFR molecules need to come together to form a homodimer. These then use the molecule of ATP to trans-phosphorylate each other on tyrosine residues, which generates phosphotyrosine residues, recruiting the phosphotyrosine-binding proteins to EGFR to assemble protein complexes that transduce signal cascades to the nucleus or activate other cellular biochemical processes. When erlotinib binds to EGFR, formation of phosphotyrosine residues in EGFR is not possible and the signal cascades are not initiated.
