 | ||
Cell therapy (also called cellular therapy or cytotherapy) is therapy in which cellular material is injected into a patient; this generally means intact, living cells. For example, T cells capable of fighting cancer cells via cell-mediated immunity may be injected in the course of immunotherapy.
Contents
- Background
- Allogeneic Cell Therapy
- Human embryonic stem cells
- Mechanisms of Action
- Neural Stem Cell Therapy
- Mesenchymal Stem Cell Therapy
- Hematopoietic stem cell transplantation
- In alternative medicine
- References
Cell therapy originated in the nineteenth century when scientists experimented by injecting animal material in an attempt to prevent and treat illness. Although such attempts produced no positive benefit, further research found in the mid twentieth century that human cells could be used to help prevent the human body rejecting transplanted organs, leading in time to successful bone marrow transplantation.
Today two distinct categories of cell therapy are recognized.
The first category is cell therapy in mainstream medicine. This is the subject of intense research and the basis of potential therapeutic benefit. Such research can be controversial when it involves human embryonic material.
The second category is in alternative medicine, and perpetuates the practice of injecting animal materials in an attempt to cure disease. This practice, according to the American Cancer Society, is not backed by any medical evidence of effectiveness, and can have deadly consequences.
Background
Cell therapy can be defined as therapy in which cellular material is injected into a patient.
There are two branches of cell therapy: one is legitimate and established, whereby human cells are transplanted from a donor to a patient; the other is dangerous alternative medicine, whereby injected animal cells are used to attempt to treat illness.
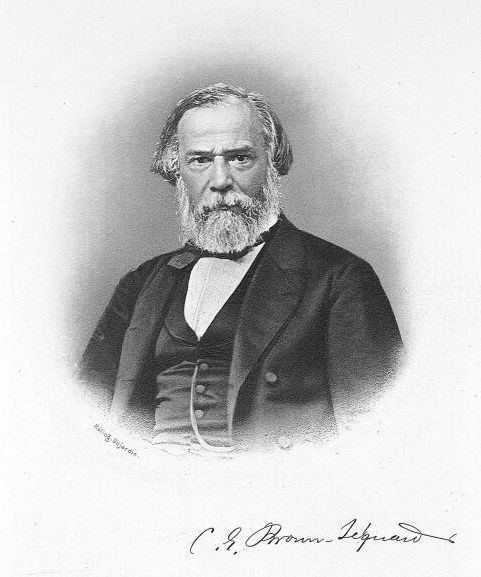
The origins of cell therapy can perhaps be traced to the nineteenth century, when Charles-Édouard Brown-Séquard (1817–1894) injected animal testicle extracts in an attempt to stop the effects of aging. In 1931 Paul Niehans (1882–1971) – who has been called the inventor of cell therapy – attempted to cure a patient by injecting material from calf embryos. Niehans claimed to have treated many people for cancer using this technique, though his claims have never been validated by research.
In 1953 researchers found that laboratory animals could be helped not to reject organ transplants by pre-inoculating them with cells from donor animals; in 1968, in Minnesota, the first successful human bone marrow transplantation took place.
Bone marrow transplants have been found to be effective, along with some other kinds of human cell therapy – for example in treating damaged knee cartilage. In recent times, cell therapy using human material has been recognized as an important field in the treatment of human disease. The experimental field of Stem cell therapy has shown promise for new types of treatment.
In mainstream medicine, cell therapy is supported by a distinct healthcare industry which sees strong prospects for future growth.
Allogeneic Cell Therapy
In allogeneic cell therapy the donor is a different person to the recipient of the cells. In pharmaceutical manufacturing, the allogenic methodology is promising because unmatched allogenic therapies can form the basis of "off the shelf" products. There is research interest in attempting to develop such products to treat conditions including Crohn's disease and a variety of vascular conditions.
Human embryonic stem cells
Research into human embryonic stem cells is controversial, and regulation varies from country to country, with some countries banning it outright. Nevertheless, these cells are being investigated as the basis for a number of therapeutic applications, including possible treatments for diabetes and Parkinson's disease.
Mechanisms of Action
Cell therapy is targeted at many clinical indications in multiple organs and by several modes of cell delivery. Accordingly, the specific mechanisms of action involved in the therapies are wide ranging. However, there are two main principles by which cells facilitate therapeutic action:
- Stem cell or progenitor cell engraftment, differentiation, and long term replacement of damaged tissue. In this paradigm multipotent or unipotent cells differentiate into a specific cell type in the lab or after reaching the site of injury (via local or systemic administration). These cells then integrate into the site of injury, replacing damaged tissue, and thus facilitate improved function of the organ or tissue. An example of this is the use of cells to replace cardiomyocytes after myocardial infarction.
- Cells that have the capacity to release soluble factors such as cytokines, chemokines, and growth factors which act in a paracrine or endocrine manner. These factors facilitate self-healing of the organ or region. The delivered cells (via local or systemic administration) remain viable for a relatively short period (days-weeks) and then die. This includes cells that naturally secrete the relevant therapeutic factors, or which undergo epigenetic changes or genetic engineering that causes the cells to release large quantities of a specific molecule. Examples of this include cells that secrete factors which facilitate angiogenesis, anti-inflammation, and anti-apoptosis. This mode of action is proposed by companies such as Pluristem and Pervasis that use adherent stromal cells or mature endothelial cells to treat peripheral artery disease and arteriovenous access complications.
Neural Stem Cell Therapy
Neural stem cells (NSCs) are the subject of ongoing research for possible therapeutic applications, for example for treating a number of neurological disorders such as Parkinson's disease and Huntington's disease.
Mesenchymal Stem Cell Therapy
MSCs are immunomodulatory, multipotent and fast proliferating and these unique capabilities mean they can be used for a wide range of treatments including immune-modulatory therapy, bone and cartilage regeneration, myocardium regeneration and the treatment of Hurler syndrome, a skeletal and neurological disorder.
Researchers have demonstrated the use of MSCs for the treatment of osteogenesis imperfecta (OI). Horwitz et al. transplanted bone marrow (BM) cells from human leukocyte antigen (HLA)-identical siblings to patients suffering from OI. Results show that MSCs can develop into normal osteoblasts, leading to fast bone development and reduced fracture frequencies. A more recent clinical trial showed that allogeneic fetal MSCs transplanted in utero in patients with severe OI can engraft and differentiate into bone in a human fetus.
Besides bone and cartilage regeneration, cardiomyocyte regeneration with autologous BM MSCs has also been reported recently. Introduction of BM MSCs following myocardial infarction (MI) resulted in significant reduction of damaged regions and improvement in heart function. Clinical trials for treatment of acute MI with Prochymal by Osiris Therapeutics are underway. Also, a clinical trial revealed huge improvements in nerve conduction velocities in Hurler’s Syndrome patients infused with BM MSCs from HLA-identical siblings.
Hematopoietic stem cell transplantation
HSCs possess the ability to self-renew and differentiate into all types of blood cells, especially those involved in the human immune system. Thus, they can be used to treat blood and immune disorders. Since human bone marrow (BM) grafting was first published in 1957, there have been significant advancements in HSCs therapy. Following that, syngeneic marrow infusion and allogeneic marrow grafting were performed successfully. HSCs therapy can also render its cure by reconstituting damaged blood-forming cells and restoring the immune system after high-dose chemotherapy to eliminate disease.
There are three types of HSCT: syngeneic, autologous, and allogeneic transplants. Syngeneic transplantations occur between identical twins. Autologous transplantations use the HSCs obtained directly from the patient and hence do not cause any complications of tissue incompatibility; whereas allogeneic transplantations involve the use of donor HSCs, either genetically related or unrelated to the recipient. To lower the risks of transplant, which include graft rejection and Graft-Versus-Host Disease (GVHD), allogeneic HSCT must satisfy compatibility at the HLA loci (i.e. genetic matching to reduce the immunogenicity of the transplant). Mismatch of HLA loci would result in treatment-related mortality and higher risk of acute GVHD.
In addition to BM derived HSCs, the use of alternative sources such as umbilical cord blood (UCB) and peripheral blood stem cells (PBSCs) has been increasing. In comparison with BM derived HSCs recipients, PBSCs recipients afflicted with myeloid malignancies reported a faster engraftment and better overall survival. However, this was at the expense of increased rate of GVHD. Also, the use of UCB requires less stringent HLA loci matching, although the time of engraftment is longer and graft failure rate is higher.
In alternative medicine
In alternative medicine, cell therapy is defined as the injection of non-human cellular animal material in an attempt to treat illness. Quackwatch labels this as "senseless", since "cells from the organs of one species cannot replace the cells from the organs of other species" and because a number of serious adverse effects have been reported.
Of this alternative, animal-based form of cell therapy, the American Cancer Society say: "Available scientific evidence does not support claims that cell therapy is effective in treating cancer or any other disease. In may in fact be lethal ...".
