Synonyms Capgras syndrome Specialty Psychiatry MeSH D002194 | Pronunciation /kæpˈɡrɑː/ kap-GRAH DiseasesDB 32606 | |
Capgras delusion is a disorder in which a person holds a delusion that a friend, spouse, parent, or other close family member (or pet) has been replaced by an identical-looking impostor. The Capgras delusion is classified as a delusional misidentification syndrome, a class of delusional beliefs that involves the misidentification of people, places, or objects (usually not in conjunction). It can occur in acute, transient, or chronic forms. Cases in which patients hold the belief that time has been "warped" or "substituted" have also been reported.
Contents
The delusion most commonly occurs in patients diagnosed with paranoid schizophrenia, but has also been seen in patients suffering from brain injury and dementia. It presents often in individuals with a neurodegenerative disease, particularly at an older age. It has also been reported as occurring in association with diabetes, hypothyroidism, and migraine attacks. In one isolated case, the Capgras delusion was temporarily induced in a healthy subject by the drug ketamine. It occurs more frequently in females, with a female:male ratio of 3:2.
Signs and symptoms
The following two case reports are examples of the Capgras delusion in a psychiatric setting:
Mrs. D, a 74-year-old married housewife, recently discharged from a local hospital after her first psychiatric admission, presented to our facility for a second opinion. At the time of her admission earlier in the year, she had received the diagnosis of atypical psychosis because of her belief that her husband had been replaced by another unrelated man. She refused to sleep with the impostor, locked her bedroom and door at night, asked her son for a gun, and finally fought with the police when attempts were made to hospitalise her. At times she believed her husband was her long deceased father. She easily recognised other family members and would misidentify her husband only.
Diane was a 28-year-old single woman who was seen for an evaluation at a day hospital program in preparation for discharge from a psychiatric hospital. This was her third psychiatric admission in the past five years. Always shy and reclusive, Diane first became psychotic at age 23. Following an examination by her physician, she began to worry that the doctor had damaged her internally and that she might never be able to become pregnant. The patient's condition improved with neuroleptic treatment but deteriorated after discharge because she refused medication. When she was admitted eight months later, she presented with delusions that a man was making exact copies of people—"screens"— and that there were two screens of her, one evil and one good. The diagnosis was schizophrenia with Capgras delusion. She was disheveled and had a bald spot on her scalp from self-mutilation.
The following case is an instance of the Capgras delusion resulting from a neurodegenerative disease:
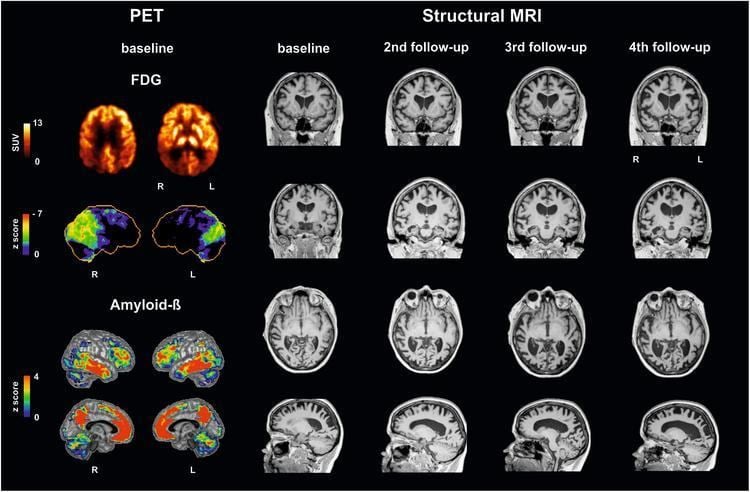
Fred, a 59-year-old man with a high school qualification, was referred for neurological and neuropsychological evaluation because of cognitive and behavioural disturbances. He had worked as the head of a small unit devoted to energy research until a few months before. His past medical and psychiatric history was uneventful. [...] Fred's wife reported that about 15 months from onset he began to see her as a "double" (her words). The first episode occurred one day when, after coming home, Fred asked her where Wilma was. On her surprised answer that she was right there, he firmly denied that she was his wife Wilma, whom he "knew very well as his sons' mother", and went on plainly commenting that Wilma had probably gone out and would come back later. [...] Fred presented progressive cognitive deterioration characterised both by severity and fast decline. Apart from CD, his neuropsychological presentation was hallmarked by language disturbances suggestive of frontal-executive dysfunction. His cognitive impairment ended up in a severe, all-encompassing frontal syndrome.
Causes
It is generally agreed that the Capgras delusion has a more complex and organic basis, and can be better understood by examining neuroanatomical damage associated with the syndrome.
The first clues to the possible causes of the Capgras delusion were suggested by the study of brain-injured patients who had developed prosopagnosia. In this condition, patients are unable to recognize faces consciously, despite being able to recognize other types of visual objects. However, a 1984 study by Bauer showed that even though conscious face recognition was impaired, patients with the condition showed autonomic arousal (measured by a galvanic skin response measure) to familiar faces, suggesting that there are two pathways to face recognition—one conscious and one unconscious.
In a 1990 paper published in the British Journal of Psychiatry, psychologists Hadyn Ellis and Andy Young hypothesized that patients with Capgras delusion may have a "mirror image" or double dissociation of prosopagnosia, in that their conscious ability to recognize faces was intact, but they might have damage to the system that produces the automatic emotional arousal to familiar faces. This might lead to the experience of recognizing someone while feeling something was not "quite right" about them. In 1997, Hadyn Ellis and his colleagues published a study of five patients with Capgras delusion (all diagnosed with schizophrenia) and confirmed that although they could consciously recognize the faces, they did not show the normal automatic emotional arousal response. The same low level of autonomic response was shown in the presence of strangers. Young (2008) has theorized that this means that patients suffering from the disease experience a "loss" of familiarity, not a "lack" of it. Further evidence for this explanation comes from other studies measuring galvanic skin responses to faces. A patient with Capgras delusion showed reduced GSRs to faces in spite of normal face recognition. This theory for the causes of Capgras delusion was summarised in Trends in Cognitive Science.
William Hirstein and Vilayanur S. Ramachandran reported similar findings in a paper published on a single case of a patient with Capgras delusion after brain injury. Ramachandran portrayed this case in his book Phantoms in the Brain, and gave a talk about it at TED 2007. Since the patient was capable of feeling emotions and recognizing faces, but could not feel emotions when recognizing familiar faces, Ramachandran hypothesizes that the origin of Capgras syndrome is a disconnection between the temporal cortex, where faces are usually recognized (see temporal lobe), and the limbic system, involved in emotions. More specifically, he emphasizes the disconnection between the amygdala and the inferotemporal cortex.
In 2010, William Hirstein revised this theory to explain why a person suffering from Capgras syndrome would have the particular reaction of not recognizing a familiar person. Hirstein explained the theory as follows:
...my current hypothesis on Capgras, which is a more specific version of the earlier position I took in the 1997 article with V. S. Ramachandran. According to my current approach, we represent the people we know well with hybrid representations containing two parts. One part represents them externally: how they look, sound, etc. The other part represents them internally: their personalities, beliefs, characteristic emotions, preferences, etc. Capgras syndrome occurs when the internal portion of the representation is damaged or inaccessible. This produces the impression of someone who looks right on the outside, but seems different on the inside, i.e., an impostor. This gives a much more specific explanation that fits well with what the patients actually say. It corrects a problem with the earlier hypothesis in that there are many possible responses to the lack of an emotion upon seeing someone.
Furthermore, Ramachandran suggests a relationship between the Capgras syndrome and a more general difficulty in linking successive episodic memories because of the crucial role emotion plays in creating memories. Since the patient could not put together memories and feelings, he believed objects in a photograph were new on every viewing, even though they normally should have evoked feelings (e.g., a person close to him, a familiar object, or even himself). Others like Merrin and Silberfarb (1976) have also proposed links between the Capgras syndrome and deficits in aspects of memory. They suggest that an important and familiar person (the usual subject of the delusion) has many layers of visual, auditory, tactile, and experiential memories associated with them, so the Capgras delusion can be understood as a failure of object constancy at a high perceptual level.
Most likely, more than an impairment of the automatic emotional arousal response is necessary to form Capgras delusion, as the same pattern has been reported in patients showing no signs of delusions. Ellis suggested that a second factor explains why this unusual experience is transformed into a delusional belief; this second factor is thought to be an impairment in reasoning, although no definitive impairment has been found to explain all cases. Many have argued for the inclusion of the role of patient phenomenology in explanatory models of the Capgras syndrome in order to better understand the mechanisms that enable the creation and maintenance of delusional beliefs.
Capgras syndrome has also been linked to reduplicative paramnesia, another delusional misidentification syndrome. Since these two syndromes are highly associated, it has been proposed that they affect similar areas of the brain and therefore have similar neurological implications. Reduplicative paramnesia is understood to affect the frontal lobe and thus it is believed that Capgras syndrome is also associated with the frontal lobe. Even if the damage is not directly to the frontal lobe, an interruption of signals between other lobes and the frontal lobe could result in Capgras syndrome.
Treatment
Individual therapy may be best suited to treat the individual's delusions. Persistence is needed in establishing a therapeutic empathy without validating the patient’s delusional system or overtly confronting the system. Cognitive techniques that include reality testing and reframing can be used. Antipsychotics and other therapeutic drugs have been used with relative success.
History
Capgras syndrome is named after Joseph Capgras (1873–1950), a French psychiatrist who first described the disorder in 1923 in his paper co-authored by Jean Reboul-Lachaux, on the case of a French woman, "Madame M.," who complained that corresponding "doubles" had taken the places of her husband and other people she knew. Capgras and Reboul-Lachaux first called the syndrome "l’illusion des sosies", which can be translated literally as "the illusion of look-alikes."
The Capgras syndrome was initially considered a purely psychiatric disorder, the delusion of a double seen as symptomatic of schizophrenia, and purely a female disorder (though this is now known not to be the case) often noted as a symptom of hysteria. Most of the proposed explanations initially following that of Capgras and Reboul-Lachaux were psychoanalytical in nature. It was not until the 1980s that attention was turned to the usually co-existing organic brain lesions originally thought to be essentially unrelated or accidental. Today, the Capgras syndrome is understood as a neurological disorder, in which the delusion primarily results from organic brain lesions or degeneration.
