Species Human Entrez 5327 | Human Mouse Ensembl ENSG00000104368 | |
 | ||
Aliases PLAT, T-PA, TPA, plasminogen activator, tissue type External IDs OMIM: 173370 MGI: 97610 HomoloGene: 717 GeneCards: PLAT | ||
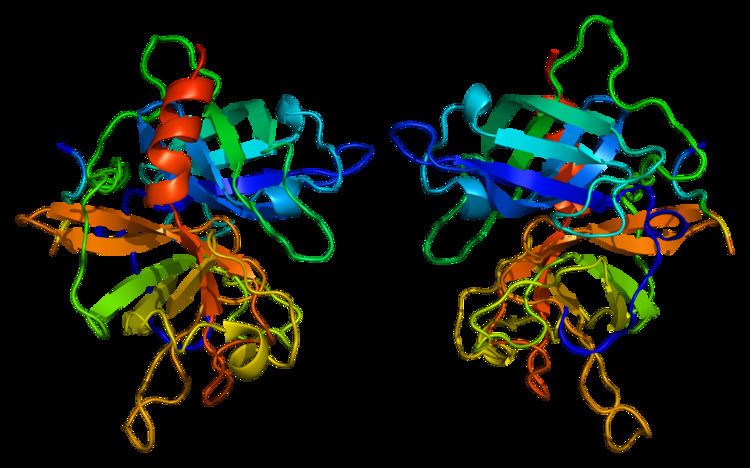
Tissue plasminogen activator (abbreviated tPA or PLAT) is a protein involved in the breakdown of blood clots. It is a serine protease (EC 3.4.21.68) found on endothelial cells, the cells that line the blood vessels. As an enzyme, it catalyzes the conversion of plasminogen to plasmin, the major enzyme responsible for clot breakdown. Because it works on the clotting system, tPA (such as alteplase, reteplase, and tenecteplase) is used in clinical medicine to treat embolic or thrombotic stroke. Use is contraindicated in hemorrhagic stroke and head trauma. The antidote for tPA in case of toxicity is aminocaproic acid.
Contents
- Tissue plasminogen activator tpa
- Medical uses
- Ischemic stroke
- Pulmonary embolism
- Recombinant tissue plasminogen activators
- Interactions
- Function
- Genetics
- Development
- References
tPA may be manufactured using recombinant biotechnology techniques. tPA created this way may be referred to as recombinant tissue plasminogen activator (rtPA). It is sold as alteplase.
Tissue plasminogen activator tpa
Medical uses
tPA is used in some cases of diseases that feature blood clots, such as pulmonary embolism, myocardial infarction, and stroke, in a medical treatment called thrombolysis. The most common use is for ischemic stroke. It can either be administered systemically, in the case of acute myocardial infarction, acute ischemic stroke, and most cases of acute massive pulmonary embolism, or administered through an arterial catheter directly to the site of occlusion in the case of peripheral arterial thrombi and thrombi in the proximal deep veins of the leg.
Ischemic stroke
There have been twelve large scale, high-quality trials of rtPA in acute ischemic stroke. A meta-analysis of these trials concluded that rtPA given within 6 hours of a stroke significantly increased the odds of being alive and independent at final follow-up, particularly in patients treated within 3 hours. However, there was an excess of mortality in treated patients in the first week after the event, mostly from intracranial haemorrhage at 7 days but mortality at final follow up was not significant between treated and untreated patients.
It has been suggested that if tPA is effective in ischemic stroke, it must be administered as early as possible after the onset of stroke symptoms. Indeed, tPA has become widely considered standard of care in acute ischemic stroke, so long as the patient presents soon after the onset of stroke symptoms. Many national guidelines including the AHA have interpreted this cohort of studies as suggesting that there are specific subgroups who may benefit from tPA and thus recommend its use within a limited time window after the event. Protocol guidelines require its use intravenously within the first three hours of the event, after which its detriments may outweigh its benefits. For example, the Canadian Stroke Network guideline states "All patients with disabling acute ischemic stroke who can be treated within 4.5 hours of symptom onset should be evaluated without delay to determine their eligibility for treatment" with tPA. Delayed presentation to the ED leads to decreased eligibility; as few as 3% of people qualify for this treatment. Similarly in the United States, the window of administration used to be 3 hours from onset of symptoms, but the newer guidelines also recommend use up to 4.5 hours after symptom onset. tPA appears to show benefit not only for large artery occlusions but also for lacunar strokes. Since tPA dissolves blood clots, there is risk of hemorrhage with its use.
Use of tPA in the United States in treatment of patients who are eligible for its use, no contra-indications and arrival at the treating facility less than 3 hours after onset of symptoms, is reported to have doubled from 2003 to 2011. Use on patients with mild deficits, of nonwhite race/ethnicity, and oldest old age increased. However, many patients who were eligible for treatment were not treated.
tPA has also been given to patients with acute ischemic stroke above age 90 years old. Although a small fraction of patients 90 years and above treated with tPA for acute ischemic stroke recover, most patients have a poor 30-day functional outcome or die. Nonagenarians may do as well as octogenarians following treatment with IV-tPA for acute ischemic stroke. In addition, people with frostbite treated with tPA had fewer amputations than those not treated with tPA.
There is consensus amongst stroke specialists that tPA is the standard of care for eligible stroke patients and benefits outweigh the risks. There is significant debate mainly in the emergency medicine community regarding recombinant tPA's effectiveness in ischemic stroke. The NNT Group on evidence-based medicine concluded that it was inappropriate to combine these twelve trials into a single analysis, because of substantial clinical heterogeneity (i.e., variations in study design, setting, and population characteristics). Examining each study individually, the NNT group noted that two of these studies showed benefit to patients given tPA (and that, using analytical methods that they think flawed); four studies showed harm and had to be stopped before completion; and the remaining studies showed neither benefit nor harm. On the basis of this evidence, the NNT Group recommended against the use of tPA in acute ischaemic stroke. The NNT Group notes that the case for the 3-hour time window arises largely from analysis of two trials: NINDS-2 and subgroup results from IST-3. "However, presuming that early (0-3h) administration is better than later administration (3-4.5h or 4.5-6h) the subgroup results of IST-3 suggest an implausible biological effect in which early administration is beneficial, 3-4.5h administration is harmful, and 4.5-6h administration is again beneficial." Indeed, even the original publication of the IST-3 trial found that time-window effects were not significant predictors of outcome (p=0.61). In the UK, concerns by stroke specialists have led to a review by the Medicines and Healthcare products Regulatory Agency.
Pulmonary embolism
Pulmonary embolism (blood clots that have moved to the lung arteries) is usually treated with heparin generally followed by warfarin. If pulmonary embolism causes severe instability due to high pressure on the heart ("massive PE") and leads to low blood pressure, recombinant tPA is recommended.
Recombinant tissue plasminogen activators
Recombinant tissue plasminogen activators (r-tPAs) include alteplase, reteplase, and tenecteplase (TNKase).
Activase (Alteplase) is FDA-approved for treatment of myocardial infarction with ST-elevation (STEMI), acute ischemic stroke (AIS), acute massive pulmonary embolism, and central venous access devices (CVAD).
Reteplase is FDA-approved for acute myocardial infarction, where it has more convenient administration and faster thrombolysis than alteplase. This is because it is a second generation engineered TPA, hence its half life is up to 20 minutes which allows it to be administered as a bolus injection rather than an infusion like Alteplase.
Tenecteplase is also indicated in acute myocardial infarction, showing fewer bleeding complications but otherwise similar mortality rates after one year compared to alteplase.
Additional r-tPAs, such as desmoteplase, are under clinical development.
Interactions
Tissue plasminogen activator has been shown to interact with:
Function
tPA and plasmin are the key enzymes of the fibrinolytic pathway in which tPA mediated plasmin generation occurs. To be specific, tPA cleaves the zymogen plasminogen at its Arg561 - Val562 peptide bond, into the serine protease plasmin.
Increased enzymatic activity causes hyperfibrinolysis, which manifests as excessive bleeding and/or an increase of the vascular permeability. Decreased activity leads to hypofibrinolysis which can result in thrombosis or embolism. In ischemic stroke patients, decreased tPA activity was reported to be associated with an increase in plasma P-selectin concentration.
Tissue plasminogen activator also plays a role in cell migration and tissue remodeling.
Genetics
Tissue plasminogen activator is a protein encoded by the PLAT gene, which is located on chromosome 8. The primary transcript produced by this gene undergoes alternative splicing, producing three distinct messenger RNAs.
Development
tPA was first produced by recombinant DNA techniques at Genentech in 1982.
