Pregnancycategory TBD ATC code L01XX51 (WHO) CAS Number 1187560-31-1 | Routes ofadministration Injection Legal status US: ℞-only ChemSpider none | |
 | ||
Talimogene laherparepvec (tal im' oh jeen la her" pa rep' vek), (T-Vec, tradenamed Imlygic, formerly called OncoVexGM-CSF) is a biopharmaceutical drug to treat melanoma lesions that cannot be operated on; it is injected directly into the lesion. As of 2016 there was no evidence that it extends the life of people with melanoma, or that it prevents metastasis.
Contents
Around half of people treated with T-Vec in clinical trials experienced fatigue and chills; around 40% had fever, around 35% had nausea, and around 30% had flu-like symptoms as well as pain at the injection site. The reactions were mild to moderate in severity; 2% of people had severe reactions and these were generally cellulitis.
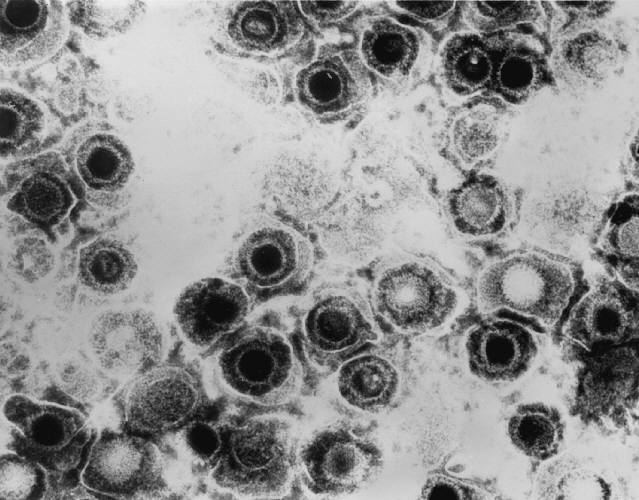
T-Vec is a genetically engineered herpes virus (an oncolytic herpes virus). Two genes were removed – one that shuts down an individual cell's defenses, and another that helps the virus evade the immune system –, and a gene for human GM-CSF was added. The drug works by replicating in cancer cells, causing them to burst; it was also designed to stimulate an immune response but as of 2016, there was no evidence of this.
The drug was created and initially developed by BioVex, Inc. and was continued by Amgen, which acquired BioVex in 2011. It was the first oncolytic virus approved in the West; it was approved in the US in October 2015 and provisionally approved in Europe in December 2015.
Medical uses
T-Vec is delivered locally by injecting it directly into melanoma lesions.
In the US and Europe, T-Vec is used to treat melanoma lesions that cannot be operated on that are on or in the skin it is injected directly into the lesion; the population is more restricted in Europe.
It has not been proven to extend survival nor to prevent metastases.
The drug should not be used for people with very weak immune system. Women should take precautions not to become pregnant while taking T-Vec and pregnant and nursing women should not take it.
Adverse effects
Around half of people treated with T-Vec in clinical trials experienced fatigue and chills; around 40% had fever, around 35% had nausea, and around 30% had flu-like symptoms as well as pain at the injection site. The reactions were mild to moderate in severity; 2% of people had severe reactions and these were generally cellulitis.
More than 10% of people had edema, headache, cough, vomiting, diarrhea, constipation, muscle pain, or joint pain. Between 1% and 10% developed cold sores, pain or infection in the lesion, anemia, immune mediated events (like vasculitis, pneumonia, worsening psoriasis, or glomerulonephritis), dehydration, confusion, anxiety, depression, dizziness, insomnia, ear pain, fast heart beating, deep vein thrombosis, high blood pressure, flushing, shortness of breath when exercising, sore throat, symptoms of the common cold, stomach pain, back pain, groin pain, weight loss, or oozing from the injection site.
Like wild herpes simplex virus, T-Vec may persist in neurons exposed to it, and it may cause latent infections.
Pharmacology
T-Vec is taken up by normal cells and cancer cells like the wild type herpes simplex virus, it is cleared in the same way. Bioavailability and systemic concentrations have not been measured since the drug replicates once it is injected.
Mechanism
T-Vec directly destroys the cancer cells it infects; it was also designed to stimulate an immune response but as of 2016, there was no evidence of this.
The virus invades both cancerous and healthy cells, but it cannot replicate in healthy cells because it lacks Infected cell protein 34.5 (ICP34.5). When cells are infected with a virus they shut down and die, but ICP34.5 blocks this stress response, allowing the virus to hijack the cell's translation machinery to replicate itself. A herpesvirus lacking the gene coding for ICP34.5 cannot replicate in normal cells. However, in many cancer cells the stress response is already disrupted, so a virus lacking ICP34.5 can still replicate in them. After the virus has replicated many times, the cell swells and finally bursts, killing the cell and releasing the copies of the virus, which can then infect nearby cells.
While T-Vec is using the cells's translation machinery to replicate, it also uses it make the cell create GM-CSF. In theory, the GM-CSF that is secreted or released when the cancer cell bursts, attracts dendritic cells to the site, which pick up the tumor antigens, process them, and then present them on their surface to cytotoxic (killer) T cells which in turn sets of an immune response. Whether GM-CSF produced from T-Vec is actually causing such an immune response in people to whom T-Vec was administered, was not certain as of 2016.
Composition
T-Vec is a biopharmaceutical drug; it is an oncolytic herpes virus that was created by genetically engineering a strain of herpes simplex virus 1 (HSV-1) taken from a person infected with the virus, rather than a laboratory strain. Both copies of the viral gene coding for ICP34.5 were deleted and replaced with the gene coding for human GM-CSF, and the gene coding for ICP47 was removed. In wild herpes virus, ICP47 suppresses the immune response to the virus; it was removed because the drug was designed with the intention of activating the immune system.
History
The first oncolytic virus to be approved by a regulatory agency was a genetically modified adenovirus named H101 by Shanghai Sunway Biotech. It gained regulatory approval in 2005 from China's State Food and Drug Administration (SFDA) for the treatment of head and neck cancer.
T-Vec was created and initially developed by BioVex, Inc. under the brand OncoVEXGM-CSF. Development was continued by Amgen, which acquired BioVex in 2011. BioVex was founded in 2000, based on research by Robert Coffin at University College London, and moved its headquarters to Woburn, Massachusetts in 2005, leaving about half its employees in the UK.
The phase II clinical trial in melanoma was published in 2009 and the phase III trial was published in 2013.
T-vec was approved by the U.S. Food and Drug Administration to treat melanoma in October 2015. It was the first approval of an oncolytic virus in the West. It was provisionally approved by the European Medicines Agency in December of that year – continued marketing approval depended on further clinical results.
Sales
Amgen estimated that T-Vec would be priced at $65,000 per patient at the time it was approved.
Research
As of 2016, T-vec had been studied in early stage clinical trials in pancreatic cancer, soft-tissue sarcoma, and head and neck squamous-cell carcinoma; it had also been tested in combination with checkpoint inhibitors ipilimumab and pembrolizumab.
