AHFS/Drugs.com Monograph Routes ofadministration IM/IV Legal status US: ℞-only | MedlinePlus a609005 ATC code J01FF02 (WHO) | |
 | ||
Pregnancycategory US: C (Risk not ruled out) | ||
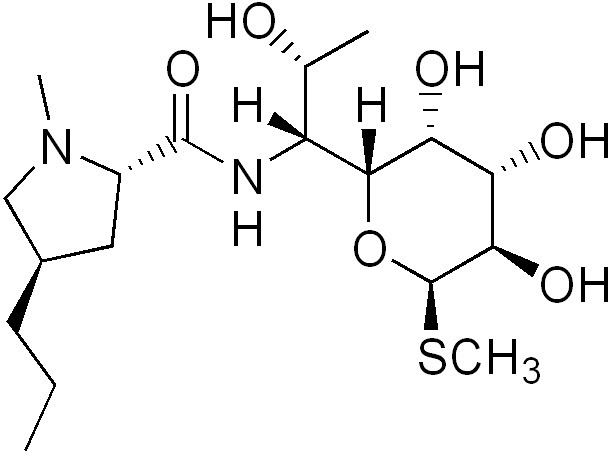
Lincomycin is a lincosamide antibiotic that comes from the actinomycete Streptomyces lincolnensis. A related compound, clindamycin, is derived from lincomycin by using thionyl chloride to replace the 7-hydroxy group with a chlorine atom with inversion of chirality.
Contents
Uses
Although similar in structure, antibacterial spectrum, and mechanism of action to macrolides, lincomycin is also effective against other organisms including actinomycetes and some species of Mycoplasma and Plasmodium.
However, because of its adverse effects and toxicity, it is rarely used today and reserved for patients allergic to penicillin or where bacteria have developed resistance.
Clinical pharmacology
Intramuscular administration of a single dose of 600 mg of Lincomycin produces average peak serum levels of 11.6 micrograms/ml at 60 minutes, and maintains therapeutic levels for 17 to 20 hours, for most susceptible gram-positive organisms. Urinary excretion after this dose ranges from 1.8 to 24.8 percent (mean: 17.3 percent).
A two-hour intravenous infusion of 600 mg of Lincomycin achieves average peak serum levels of 15.9 micrograms/ml and yields therapeutic levels for 14 hours for most susceptible gram-positive organisms. Urinary excretion ranges from 4.9 to 30.3 percent (mean: 13.8 percent).
The biological half-life after IM or IV administration is 5.4 ± 1.0 hours. The serum half-life of lincomycin may be prolonged in patients with severe impairment of renal function, compared to patients with normal renal function. In patients with abnormal hepatic function, serum half-life may be twofold longer than in patients with normal hepatic function. Hemodialysis and peritoneal dialysis are not effective in removing lincomycin from the serum.
Tissue level studies indicate that bile is an important route of excretion. Significant levels have been demonstrated in the majority of body tissues. Although lincomycin appears to diffuse in the cerebrospinal fluid (CSF), levels of lincomycin in the CSF appear inadequate for the treatment of meningitis.
Biosynthesis
Lincomycin is an antibiotic classified as a constituent of the lincosamide group, which typically feature a 6,8-dideoxy-6-aminooctose lincosamine. In Lincomycin A, this sugar moiety (referred to as methylthiolincosamide) is linked via an amide bond to an amino acid derivative (referred to as propylhygric acid). Lincomycin biosynthesis occurs via a biphasic pathway. Propylproline and methylthiolincosamide are each synthesized separately, which are then condensed to form N-demethyllincomycin and finally methylated by S-adenosyl methionine to give lincomycin.
In the biosynthesis of the amino acid moiety of lincomycin, tyrosine comprises seven of the nine carbons in the prophylhygric acid, while the remaining two carbons are added in reactions with S-adenosyl methionine. Glucose is converted via glycolysis and the hexose monophosphate pathway to phosphoenolpyruvate and erythrose-4-phosphate, respectively, which are converted via the shikimate pathway to tyrosine and dihydroxyphenylalanine. Although the multistep conversion of dihydroxyphenylalanine to propylproline remains unknown, experiments involving accumulation of 1,2,3,6-tetradehydro-propylproline in mutants lacking a reductase requiring lincomycin cosynthetic factor suggests a biosynthetic scheme that Kuo and coworkers have modified from Brahme et al. to accommodate the remaining steps leading to propylproline.
The biosynthetic pathway for production of the methythiolincosamide sugar moiety is still not entirely known, although two different pathways have been predicted. One possible pathway proposes the C8 carbon framework of methythiolincosamide originates from the condensation of a pentose (C5) unit, stemming from either the hexose monophosphate or condensation through a transketolase reaction with glyceraldehyde-3-phosphate and sedoheptulose-7-phosphate, and a C3 unit, added through a transaldolase reaction with sedoheptulose-7-phosphate. Once condensed, an octose (C8) unit is formed that can undergo isomerization to octose, dephosphorylation and reduction of the C8 carbon, transamination of 6-ketooctose, and thiomethylation of C1 to finally convert the octose unit to the methylthiolincosamide. A substantially different pathway for the formation of the methythiolincosamide proposes that its biosynthesis involves nucleotide activation followed by a series of modifications of dNTP-activated sugar intermediates. Eight genes, lmb-LMNZPOSQ, have been found to form a "sugar subcluster" which might be involved in this sugar metabolism.
Condensation of the carboxyl group on the propylproline with the amine group of the methylthiolincosamide via an amide bond is catalyzed by N-Demethyllincomycin-synthetase. The resulting N-demethyllincomycin is then methylated by S-adenosyl methionine through N-Demethyllincomycin methyl transferase to form the final lincomycin product.
Spectrum of susceptibility
Lincomycin is a narrow spectrum antibiotic with activity against Gram-positive and cell wall-less bacteria including pathogenic species of Streptococcus, Staphylococcus, and Mycoplasma. Lincomycin is used to treat severe bacterial infections in patients who cannot use penicillin antibiotics. Lincomycin shows weak activity against most Gram-negative bacteria. The following represents susceptibility (MIC) data for a few pathogenic bacteria:
