ICD-10 I25.5 | ||
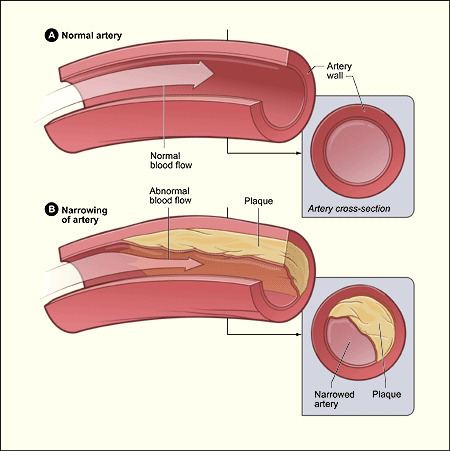 | ||
Ischemic cardiomyopathy is a type of cardiomyopathy caused by a narrowing of the coronary arteries which supply blood to the heart. Typically, patients with ischemic cardiomyopathy have a history of acute myocardial infarction, however, it may occur in patients with coronary artery disease, but without a past history of acute myocardial infarction. This cardiomyopathy is one of the leading causes of sudden cardiac death.
Contents
Signs and symptoms
Signs and symptoms of ischemic cardiomyopathy include sudden fatigue, shortness of breath, dizziness and palpitations.
Cause
Ischemic cardiomyopathy is the cause of more than 60% of all cases of systolic congestive heart failure in most countries of the world. A chest radiography that demonstrates coronary artery calcification is a probable indication of ischemic cardiomyopathy.
The following are causes of ischemic cardiomyopathy:
Pathophysiology
Ischemic cardiomyopathy is caused by too little oxygen reaching the muscular layer of the heart due to a narrowing of coronary arteries, resulting in decreased blood flow to the heart's muscular layer, in turn causing cell death. This can cause different levels of tissue injury and affect large and intermediate arteries alike.
Diagnosis
Ischemic cardiomyopathy can be diagnosed via magnetic resonance imaging (MRI) protocol, imaging both global and regional function. Also the Look-Locker technique is used to identify diffuse fibrosis; it is therefore important to be able to determine the extent of the ischemic scar. Some argue that only left main- or proximal-left anterior descending artery disease is relevant to the diagnostic criteria for ischemic cardiomyopathy. Myocardial imaging usually demonstrates left ventricular dilation, severe ventricular dysfunction, and multiple infarctions. Signs include congestive heart failure, angina edema, weight gain and fainting, among others.
Management
Restoring adequate blood flow to the heart muscle in patients with heart failure and significant coronary artery disease is strongly associated with improved survival, some research showing up to 75% survival rates over 5 years. A stem cell study indicated that using autologous cardiac stem cells as a regenerative approach for the human heart (after a heart attack) has great potential.
American Heart Association practice guidelines indicate (ICD) implantable cardioverter-defibrillator use in those with ischemic cardiomyopathy (40 days post-MI) that are (NYHA) New York Heart Association functional class I. LVEF of >30% is often used to differentiate primary from ischemic cardiomyopathy, and a prognostic indicator. At the same time, patients who undergo ventricular restoration on top of coronary artery bypass show improved postoperative ejection fraction as compared to those treated with only coronary artery bypass surgery. Severe cases are treated with heart transplantation.
Prognosis
One of the most important features differentiating ischemic cardiomyopathy from the other forms of cardiomyopathy is the shortened, or worsened all-cause mortality in patients with ischemic cardiomyopathy. According to several studies, coronary artery bypass graft surgery has a survival advantage over medical therapy (for ischemic cardiomyopathy) across varied follow-ups.
