ICD-9-CM 37.51 MedlinePlus 003003 | MeSH D016027 | |
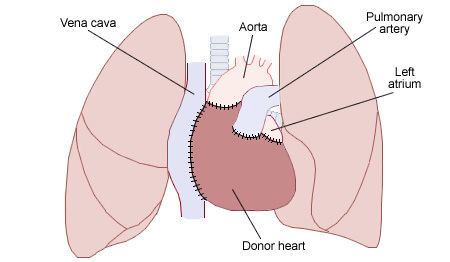 | ||
A heart transplant, or a cardiac transplant, is a surgical transplant procedure performed on patients with end-stage heart failure or severe coronary artery disease when other medical or surgical treatments have failed. As of 2016, the most common procedure is to take a functioning heart (with or without transplantation of a lung or lungs; a cadaveric donor cardiectomy) from a recently deceased organ donor (the cadaveric allograft), and implant it into the patient. The patient's own heart is either removed (the cardiectomy for the recipient) and replaced with the donor heart (orthotopic procedure) or, less commonly, the recipient's diseased heart is left in place to support the donor heart (heterotopic procedure). Approximately 3500 heart transplants are performed every year in the world, more than half of which occur in the US. Post-operation survival periods average 15 years. Heart transplantation is not considered to be a cure for heart disease, but a life-saving treatment intended to improve the quality of life for recipients.
Contents
History
One of the first mentions of the possibility of heart transplantation was by American medical researcher Simon Flexner, who declared in a reading of his paper on “Tendencies in Pathology” in the University of Chicago in 1907 that it would be possible in the then-future for diseased human organs substitution for healthy ones by surgery — including arteries, stomach, kidneys and heart.
Norman Shumway is widely regarded as the father of heart transplantation although the world's first adult human heart transplant was performed by a South African cardiac surgeon, Christiaan Barnard, utilizing the techniques developed and perfected by Shumway and Richard Lower. Barnard performed the first transplant on Louis Washkansky on December 3, 1967, at the Groote Schuur Hospital in Cape Town, South Africa. Adrian Kantrowitz performed the world's first pediatric heart transplant on December 6, 1967, at Maimonides Hospital in Brooklyn, New York, barely three days after Christiaan Barnard's pioneering operation. Since the 19-day-old infant died little more than six hours after receiving the heart, this operation was considered a failure.Norman Shumway performed the first adult heart transplant in the United States on January 6, 1968, at the Stanford University Hospital.
On 9 June 1984 “JP” Lovette IV of Denver became the world’s first successful pediatric heart transplant. Columbia-Presbyterian Medical Center surgeons transplanted the heart of 4-year-old John Nathan Ford of Harlem into 4-year-old JP a day after the Harlem child died of injuries received in a fall from a fire escape at his home. JP was born with multiple heart defects. The transplant was done by a surgical team led by Dr. Eric A. Rose, director of cardiac transplantation at NewYork–Presbyterian Hospital. Drs. Keith Reemtsma and Fred Bowman also were members of the team for the six-hour operation.
Worldwide, about 3,500 heart transplants are performed annually. The vast majority of these are performed in the United States (2,000–2,300 annually). Cedars-Sinai Medical Center in Los Angeles, California, currently is the largest heart transplant center in the world, having performed 132 adult transplants in 2015 alone. About 800,000 people have NYHA Class IV heart failure symptoms indicating advanced heart failure. The great disparity between the number of patients needing transplants and the number of procedures being performed spurred research into the transplantation of non-human hearts into humans after 1993. Xenografts from other species and artificial hearts are two less successful alternatives to allografts.
Most published surgical methods of HT necessarily divide the Vagus nerve and thus amputate parasympathetic control of the myocardium.
Contraindications
Some patients are less suitable for a heart transplant, especially if they suffer from other circulatory conditions related to their heart condition. The following conditions in a patient increase the chances of complications;
Absolute contraindications:
Relative contraindications:
Patients who are in need of a heart transplant but do not qualify, may be candidates for an artificial heart or a left ventricular assist device i.e. LVAD.
Complications
Post-operative complications include infection, sepsis, organ rejection, as well as the side-effects of the immunosuppressive medication. Since the transplanted heart originates from another organism, the recipient's immune system typically attempts to reject it. The risk of rejection never fully goes away, and the patient will be on immunosuppressive drugs for the rest of his or her life, but these may cause unwanted side effects, such as increased likelihood of infections or development of certain cancers. Recipients can acquire kidney disease from a heart transplant due to side effects of immunosuppressant medications. Many recent advances in reducing complications due to tissue rejection stem from mouse heart transplant procedures. Surgery death rate is 5-10% in 2011.
Prognosis
The prognosis for heart transplant patients following the orthotopic procedure has increased over the past 20 years, and as of June 5, 2009, the survival rates were:
In a study spanning 1999 to 2007, conducted on behalf of the U.S. federal government by Dr. Eric Weiss of the Johns Hopkins University School of Medicine, it was discovered that, compared to men receiving male hearts, "men receiving female hearts had a 15% increase in the risk of adjusted cumulative mortality" over five years. No significant differences were noted with females receiving hearts from male or female donors.
