 | ||
Immunoglobulin G (IgG) is a type of antibody. Each IgG has two antigen binding sites. Representing approximately 75% of serum antibodies in humans, IgG is the most common type of antibody found in the circulation. IgG molecules are created and released by plasma B cells.
Contents
Functions
Antibodies are major components of humoral immunity. IgG is the main type of antibody found in blood and extracellular fluid allowing it to control infection of body tissues. By binding many kinds of pathogens such as viruses, bacteria, and fungi, IgG protects the body from infection.
It does this through several mechanisms:
IgG antibodies are generated following class switching and maturation of the antibody response and thus participate predominantly in the secondary immune response. IgG is secreted as a monomer that is small in size allowing it to easily perfuse tissues. It is the only isotype that has receptors to facilitate passage through the human placenta, thereby providing protection to the fetus in utero. Along with IgA secreted in the breast milk, residual IgG absorbed through the placenta provides the neonate with humoral immunity before its own immune system develops. Colostrum contains a high percentage of IgG, especially bovine colostrum. In individuals with prior immunity to a pathogen, IgG appears about 24–48 hours after antigenic stimulation.
Therefore, in the first six months of life, the fetus has the same antibodies as the mother, till the old antibodies are then degraded and he can defend himself against all the pathogens that the mother encountered in her life (even if only through vaccination). This repertoire of immunoglobulins is crucial for the newborns who are very sensitive to infections above all for the respiratory and digestive systems.
IgG are also involved in the regulation of allergic reactions. According to Finkelman, there are two pathways of systemic anaphylaxis: antigens can cause systemic anaphylaxis in mice through classic pathway by cross-linking IgE bound the mast cell FcεRI, stimulating the release of both histamine and platelet activating factor (PAF). In the Alternative pathway antigens form complexes with IgG, which then cross-link macrophage FcγRIII and stimulates only PAF release.
IgG antibodies can prevent IgE mediated anaphylaxis by intercepting a specific antigen before it binds to mast cell –associated IgE. Consequently, IgG antibodies block systemic anaphylaxis induced by small quantities of antigen but can mediate systemic anaphylaxis induced by larger quantities.
Structure
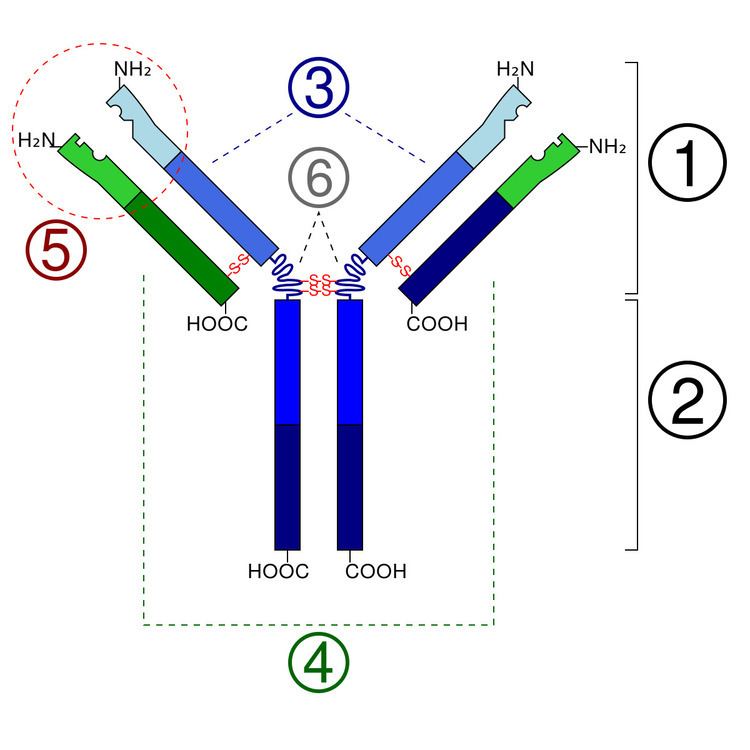
IgG antibodies are large molecules of about 150 kDa made of four peptide chains. It contains two identical class γ heavy chains of about 50 kDa and two identical light chains of about 25 kDa, thus a tetrameric quaternary structure. The two heavy chains are linked to each other and to a light chain each by disulfide bonds. The resulting tetramer has two identical halves, which together form the Y-like shape. Each end of the fork contains an identical antigen binding site. The various regions and domains of a typical IgG are depicted in the figure to the left. The Fc regions of IgGs bear a highly conserved N-glycosylation site. The N-glycans attached to this site are predominantly core-fucosylated diantennary structures of the complex type. In addition, small amounts of these N-glycans also bear bisecting GlcNAc and α-2,6-linked sialic acid residues.
Subclasses
There are four IgG subclasses (IgG1, 2, 3, and 4) in humans, named in order of their abundance in serum (IgG1 being the most abundant).
Note: IgG affinity to Fc receptors on phagocytic cells is specific to individual species from which the antibody comes as well as the class. The structure of the hinge regions (region 6 in the diagram) contributes to the unique biological properties of each of the four IgG classes. Even though there is about 95% similarity between their Fc regions, the structure of the hinge regions is relatively different.
Given the opposing properties of the IgG subclasses (fixing and failing to fix complement; binding and failing to bind FcR), and the fact that the immune response to most antigens includes a mix of all four subclasses, it has been difficult to understand how IgG subclasses can work together to provide protective immunity. Recently the Temporal Model of human IgE and IgG function was proposed. This model suggests that IgG3 (and IgE) appear early in a response. The IgG3, though of relatively low affinity, allows IgG-mediated defences to join IgM-mediated defences in clearing foreign antigens. Subsequently, higher affinity IgG1 and IgG2 are produced. The relative balance of these subclasses, in any immune complexes that form, helps determine the strength of the inflammatory processes that follow. Finally, if antigen persists, high affinity IgG4 is produced, which dampens down inflammation by helping to curtail FcR-mediated processes.
The relative ability of different IgG subclasses to fix complement may explain why some anti-donor antibody responses do harm a graft after organ transplantation.
In a mouse model of autoantibody mediated anemia using IgG isotype switch variants of an anti erythrocytes autoantibody, it was found that mouse IgG2a was superior to IgG1 in activating complement. Moreover, it was found that the IgG2a isotype was able to interact very efficiently with FcgammaR. As a result, 20 times higher doses of IgG1, in relationship to IgG2a autoantibodies, were required to induce autoantibody mediated pathology. It is important to remember that mouse IgG1 and human IgG1 are not necessarily similar in function, and the inference of human antibody function from mouse studies must be done with great care. Nevertheless, it remains true that both human and mouse antibodies have different abilities to fix complement and to bind to Fc receptors.
Use as diagnostic
The measurement of immunoglobulin G can be a diagnostic tool for certain conditions, such as autoimmune hepatitis, if indicated by certain symptoms. Clinically, measured IgG antibody levels are generally considered to be indicative of an individual's immune status to particular pathogens. A common example of this practice are titers drawn to demonstrate serologic immunity to measles, mumps, and rubella (MMR), hepatitis B virus, and varicella (chickenpox), among others.
Testing of IgG is not indicated for diagnosis of allergy.
Use in therapy
IgG antibodies are extracted from donated blood plasma and used as a therapeutic known as intravenous immunoglobulin therapy (IVIG). This is used to treat immune deficiencies, autoimmune disorders, and infections.
