Specialty oncology | ||
 | ||
ICD-10 C09.0-C10.9C01,C02.4,C14.2 | ||
Human papillomavirus (HPV)-positive oropharyngeal cancer (OPC) also known as HPV16+ oropharyngeal cancer or HPV+ OPC is a recognized subtype of oropharyngeal squamous cell carcinomas (OSCC), associated with the HPV type 16 virus.
Contents
Causes
HPV oral infection precedes the development of HPV+ OPC. Slight injuries in the mucous membrane serve as an entry gate for HPV, which thus works into the basal layer of the epithelium. People testing positive for HPV16 oral infection have a 14 times increased risk of developing HPV+ OPC.
Immunosuppression seems to be an increased risk factor for HPV+ OPC. Individuals with TGF-β1 genetic variations, specially T869C, are more likely to have HPV16+ OPC. TGF-β1 plays an important role in controlling the immune system.
A 1993 study has found that patients with human papillomavirus (HPV)-associated anogenital cancers had a 4.3-fold increased risk of tonsillar squamous-cell carcinoma.
Although evidence suggests that HPV16 is the main cause of OPC between non-smokers and non-drinkers, the degree to which tobacco and/or alcohol use may contribute to increase the risk of HPV+ OPC is unclear.
Concomitant human herpesvirus-8 infection can potentiate the effects of HPV-16.
Mechanism
A prospective study has found that increased HPV+ OPC risk was observed more than 15 years after HPV exposure, pointing to a slow development of the disease, like in cervical cancer.
HPV associated cancers are caused by the expression of HPV's E6 and E7 proteins that bind to and inactivate tumor suppressor proteins p53 and retinoblastoma protein (pRB), respectively, leading to malignant transformation of HPV infected cells.
The biology of HPV+ OPC is distinct of HPV- OPC with P53 degradation (inactivated by E6 instead of by genetic mutation), pRB pathway inactivation (by E7 instead of Cyclin D1 amplification), and P16 upregulation (over-expression of p16 instead of inactivation due to reduced negative feedback from pRB).
The tonsils epithelia (palatine and lingual) share similar nonkeratinization characteristics with the cervix, where HPV infection play the major role in cases of cervical cancer.
Diagnosis
HPV+ OPC is usually diagnosed at a more advanced stage than HPV- OPC.
Genetic signatures of HPV+ and HPV- OPC are different.
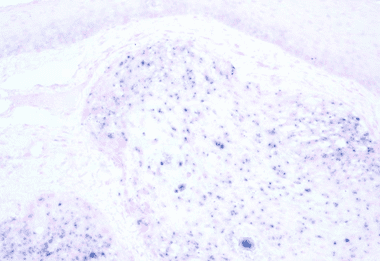
HPV OPC is associated with expression level of the E6/E7 mRNAs and of p16. Nonkeratinizing squamous cell carcinoma strongly predicts HPV-association.
HPV OPC is not merely characterized by the presence of HPV-16. Only the expression of viral oncogenes within the tumor cells plus the serum presence of E6 or E7 antibodies is unambiguously conclusive.
There's not a standard HPV testing method in head and neck cancers, both in situ hybridization and PCR are commonly used. A 2010 study has concluded that both have comparable performance for HPV detection, however it is important to use appropriate sensitivity controls.
Prevention
Risk factors are high number of sexual partners, (25% increase >= 6 partners) history of oral-genital sex, (125% >= 4 partners) history of anal–oral sex, female partner had a history of either an abnormal Pap smear or a cervical dysplasia, chronic periodontitis, and, among men, decreasing age at first intercourse and history of genital warts.
A 2010 study concluded that current tobacco users with advanced HPV+ OSCC are at higher risk of disease recurrence compared with never-tobacco users.
HPV vaccines have a theoretical potential to prevent oral HPV infection.
A 2010 review study has found that HPV16 oral infection was rare (1.3%) among the 3,977 healthy subjects analyzed.
Treatment
Currently HPV+ OPC are treated similarly to stage-matched and site-matched unrelated OPC. However less intensive use of radiotherapy or chemotherapy, as well as specific therapy, is under research.
It is hypothesized that HPV+ OPC patients benefit better from radiotherapy and concurrent cetuximab treatment than HPV- OPC patients receiving the same treatment.
Prognosis
Tumor HPV status is strongly associated with positive therapeutic response and survival compared with HPV-negative OPC. A possible explanation is "the lower probability of occurrence of 11q13 gene amplification, which is considered to be a factor underlying faster and more frequent recurrence of the disease" Presence of TP53 mutations, a marker for HPV- OPC, is associated with worse prognosis.
High grade of p16 staining is thought to be better than HPV PCR analysis in predicting radiotherapy response.
Epidemiology
HPV+ OPC patients tend to be younger than HPV- patients. Currently in the US there is a growing incidence of HPV associated oropharyngeal cancers, perhaps as a result of changing sexual behaviors, decreased popularity of tonsillectomies, improved radiologic and pathologic evaluation, and changes in classification. Tonsil and oropharyngeal cancers increased in male predominance between 1975 and 2004, despite reductions in smoking. The decline in smoking may be linked to the decreasing proportion of HPV negative cancers, while changes in sexual activity may be reflected in increasing proportion of HPV positive cancers. Recently, in the US, HPV associated OPC represent about 60% of OPC cases compared with 40% in the previous decade. By 2007, in the US, incidence of general OPC, including non-HPV associated, is 3.2 cases per 100,000 males/year and 1.9 per 100,000 all-sexes/year.
The higher increase incidence of HPV associated OPC is also seen in other countries, like Sweden, with a 2007 incidence of over 80% for cancer in the tonsils, Finland and Czech Republic. Partners of patients with HPV positive oropharyngeal cancer do not seem to have elevated oral HPV infection compared with the general population. In Australia incidence of HPV associated OPC is 1.56 cases per 100,000 males/year.
History
In 1983, it was first suggested that HPV might be the agent involved in the development of at least certain special types of oral cancers. In 2007 the World Health Organization stated HPV was a cause for oral cancers.
