 | ||
Evidence supports that male circumcision prevents HIV infection in men who have sex with women. In 2011, the WHO and the Joint United Nations Programme on HIV/AIDS (UNAIDS) stated that male circumcision could be an efficacious intervention for HIV prevention if carried out by well trained medical professionals and under clean conditions. The United States Disease Control Center states that circumcision reduces the risk that a man will acquire HIV and other STIs from an infected female partner.
Contents
- Men who have sex with men
- Recommendations
- Risk
- Mechanism of action
- Hypotheses and early work
- African trials
- Society and culture
- References
A meta-analysis of data from fifteen observational studies of men who have sex with men found "insufficient evidence that male circumcision protects against HIV infection or other STIs." The CDC concludes "There are as yet no convincing data to help determine whether male circumcision will have any effect on HIV risk for men who engage in anal sex with either a female or male partner, as either the insertive or receptive partner."
Men who have sex with men
A 2008 meta-analysis of 53,567 gay and bisexual men (52% circumcised) found that the rate of HIV infection was non-significantly lower among men who were circumcised compared with those who were uncircumcised. For men who engaged primarily in insertive anal sex, a protective effect was observed, but it too was not statistically significant. Observational studies included in the meta-analysis that were conducted prior to the introduction of highly active antiretroviral therapy in 1996 demonstrated a statistically significant protective effect for circumcised MSM against HIV infection.
Recommendations
In 2007 the World Health Organization (WHO) reviewed the evidence that had accumulated around male circumcision and HIV. The WHO and UNAIDS issued joint recommendations concerning male circumcision and HIV/AIDS. These recommendations are:
Kim Dickson, coordinator of the working group that authored the report, commented:
In 2013, WHO announced that Prepex, a non-surgical device, had been pre-qualified for the purpose of adult male circumcision for HIV prevention. The device is expected to scale up voluntary medical male circumcision in priority countries, where HIV programmes have been facing challenges due to the shortage of skilled providers performing the conventional surgical procedure. WHO further suggests that devices may have the potential to make the procedure safer, easier and quicker since it also allows other types of trained health workers (e.g. nurses) to perform the circumcision.
The World Health Organization (WHO) said: "Although these results demonstrate that male circumcision reduces the risk of men becoming infected with HIV, the UN agencies emphasize that it does not provide complete protection against HIV infection. Circumcised men can still become infected with the virus and, if HIV-positive, can infect their sexual partners. Male circumcision should never replace other known effective prevention methods and should always be considered as part of a comprehensive prevention package, which includes correct and consistent use of male or female condoms, reduction in the number of sexual partners, delaying the onset of sexual relations, and HIV testing and counselling."
Others have also expressed concern that some may mistakenly believe they will be fully protected against HIV through circumcision and see circumcision as a safe alternative to other forms of protection, such as condoms.
Risk
If proper hygienic procedures are not adhered to, the circumcision operation itself can spread HIV. Brewer et al. (2007) report, "[circumcised] male and female virgins were substantially more likely to be HIV infected than uncircumcised virgins. Among adolescents, regardless of sexual experience, circumcision was just as strongly associated with prevalent HIV infection. However, uncircumcised adults were more likely to be HIV positive than circumcised adults." They concluded: "HIV transmission may occur through circumcision-related blood exposures in eastern and southern Africa."
An interim analysis from the Rakai Health Sciences Program in Uganda suggested that newly circumcised HIV positive men may be more likely to spread HIV to their female partners if they have sexual intercourse before the wound is fully healed. “Because the total number of men who resumed sex before certified wound healing is so small, the finding of increased transmission after surgery may have occurred by chance alone. However, we need to err on the side of caution to protect women in the context of any future male circumcision programme,” said Maria Wawer, the study's principal investigator.
Kalichman et al. (2007) argue that any protective effects circumcision could offer would be partially offset by increased HIV risk behavior, or “risk compensation" including reduction in condom use or increased numbers of sex partners. They note that circumcised men in the South African trial had 18% more sexual contacts than uncircumcised men at follow-up. They also said that because participants were given ongoing risk-reduction counseling and free condoms, it "reduced the utility of these trials for estimating the potential behavioral impact of male circumcision when implemented in a natural setting." They also criticised current models for failing to account for increased HIV risk behaviour. Increased HIV risk behaviour would mean more women would be infected which would consequently increase the risk of men. It would also mean that non-HIV STI's, which have been associated with increased HIV risk, would increase.
The relative risk of HIV infection, defined as the rate of HIV infection in circumcised divided by rate in uncircumcised men, is 0.42 (95% CI 0.31-0.57), 0.44 (0.33-0.60) and 0.43 (0.32-0.59) as reported in the publications AIDS, HIV Medicine, and AIDS and Behavior respectively. Weiss et al. report that meta-analysis of "as-treated" figures from RCTs reveals a stronger protective effect (0.35; 95% CI 0.24-0.54) than if "intention-to-treat" figures are used. Byakika-Tusiime also estimated a summary relative risk of 0.39 (0.27-0.56) for observational studies, and 0.42 (0.33-0.53) overall (including both observational and RCT data). Weiss et al. report that the estimated relative risk using RCT data was "identical" to that found in observational studies (0.42). Byakika-Tusiime states that available evidence satisfies six of Hill's criteria, and concludes that the results of her analysis "provide unequivocal evidence that circumcision plays a causal role in reducing the risk of HIV infection among men." Mills et al. conclude that circumcision is an "effective strategy for reducing new male HIV infections", but caution that consistently safe sexual practices will be required to maintain the protective effect at the population level. Weiss et al. conclude that the evidence from the trials is conclusive, but that challenges to implementation remain, and will need to be faced. Lei et al. found that the relative risk of HIV acquisition by HIV- men having sex with women was 0.30. The authors also found that circumcision did not protect against HIV infection among women.
Mechanism of action
Experimental evidence supports the theory that Langerhans cells (part of the human immune system) in foreskin may be a protective factor.
Hypotheses and early work
Valiere Alcena has said that a 1986 letter he wrote to the New York State Journal of Medicine was the first time low rates of circumcision in Africa had been linked to the high rate of HIV infection there. Aaron J. Fink, a noted advocate of circumcision, also proposed that circumcision could have a preventative role—later that year the New England Journal of Medicine published his letter, "A possible explanation for heterosexual male infection with AIDS". Alcena later said that Fink had taken his ideas and got the credit for them.
By 2000, over 40 epidemiological studies had been conducted to investigate the relationship between circumcision and HIV infection. A meta-analysis conducted by researchers at the London School of Hygiene & Tropical Medicine examined 27 studies of circumcision and HIV in sub-Saharan Africa and concluded that these showed circumcision to be "associated with a significantly reduced risk of HIV infection" that could form part of a useful public health strategy.
A 2003 systematic review from the Cochrane Collaboration was more cautious. This review of 35 observational studies concluded that while there was an association between circumcision and HIV prevention, the evidence was insufficient to support changes to public health policy. A 2005 review of 37 observational studies expressed reservations about solidity of the conclusion that could be drawn because of possible confounding factors. The authors said that instead three randomized controlled trials then underway in Africa would provide "essential evidence" about the effects of circumcision on preventing HIV.
African trials
Three randomized controlled trials were commissioned as a means to reduce the effect of any confounding factors. Trials took place in South Africa, Kenya and Uganda. Africa has a higher rate of adult HIV infection than anywhere else in the world—a 1989 study had found uncircumcised men there 8.2 times more likely to have HIV.
The first trial to publish, in 2005, was that from South Africa, named ANRS-1265 or the "Orange Farm trial". After 17 months, 20 men had contracted HIV in the circumcised group and 49 in the control group—a finding which led to cessation of the trial on ethical grounds. The trial report concluded that circumcision offered protection against HIV infection "equivalent to what a vaccine of high efficacy would have achieved". Publication sparked an increased interest in the use of circumcision for AIDS prevention in international health agencies.
The other two African trials were also halted on ethical grounds, again because those in the circumcised group had a lower rate of HIV contraction than the control group. A 2008 meta-analysis of the results of all three trials found that the risk in circumcised males was 0.44 times that in uncircumcised males, and reported that 72 circumcisions would need to be performed to prevent one HIV infection. The authors also stated that using circumcision as a means to reduce HIV infection would, on a national level, require consistently safe sexual practices to maintain the protective benefit.
These randomized controlled trials that concluded that circumcision reduces the risk of HIV were not subject to blinding and as a result are subject to observer bias. Furthermore, because these trials were stopped early, this could indicate an overestimation of the effects of intervention.
Society and culture
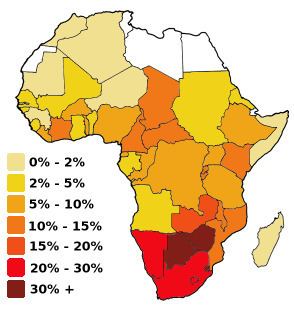
The prevalence of circumcision varies across Africa. Studies were conducted to assess the acceptability of promoting circumcision; in 2007, country consultations and planning to scale up male circumcision programmes took place in Botswana, Kenya, Lesotho, Malawi, Mozambique, Namibia, Rwanda, South Africa, Swaziland, Uganda, Tanzania, Zambia and Zimbabwe.
The UNAIDS/WHO/SACEMA Expert Group on Modelling the Impact and Cost of Male Circumcision for HIV Prevention found "large benefits" of circumcision in settings with high HIV prevalence and low circumcision prevalence. The Group estimated "one HIV infection being averted for every five to 15 male circumcisions performed, and costs to avert one HIV infection ranging from US$150 to US$900 using a 10-y time horizon". McAllister et al. estimated that consistent condom use is 95 times more cost effective than circumcision at reducing the rate of HIV in sub-Saharan Africa; the World Health Organisation states that circumcision is "highly cost-effective" in comparison to other HIV interventions when data from the South African trial are used, but less cost-effective when data from the Ugandan trial are used.
Van Howe et al. criticize the drive to promote circumcision in Africa, asking "Why are circumcision proponents expending so much time and energy promoting mass circumcision to North Americans when their supposed aim is to prevent HIV in Africa? The circumcision rate is declining in the US, especially on the west coast; the two North American national paediatric organisations have elected not to endorse the practice, and the practice’s legality has been questioned in both the medical and legal literature. ‘Playing the HIV card’ misdirects the fear understandably generated in North Americans by the HIV/AIDS pandemic into a concrete action: the perpetuation of the outdated practice of neonatal circumcision."
