ICD-10 R55 OMIM 609289 MeSH D019462 | ICD-9-CM 78Ø.2 DiseasesDB 13777 | |
 | ||
Specialty Neurologycardiovascular | ||
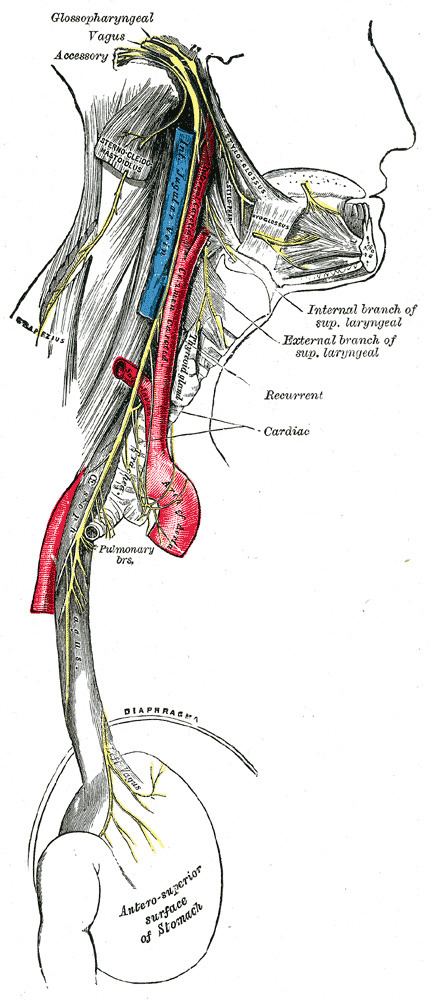
A vasovagal syncope, vasovagal episode or vasovagal response also called a neurocardiogenic syncope is a malaise mediated by the vagus nerve. Vasovagal syncope is the most common type of fainting. Vasovagal syncope is most commonly found in adolescents and in older adults.
Contents
There are different syncope syndromes which fall under the umbrella of vasovagal syncope. The common element among these conditions is the central mechanism which may lead to the loss of consciousness. The differences among them are in the factors that trigger this mechanism.
Signs and symptoms
Episodes of vasovagal syncope are typically recurrent and usually occur when the predisposed person is exposed to a specific trigger. Prior to losing consciousness, the individual frequently experiences early signs or symptoms such as lightheadedness, nausea, the feeling of being extremely hot or cold (accompanied by sweating), ringing in the ears (tinnitus), an uncomfortable feeling in the heart, fuzzy thoughts, confusion, a slight inability to speak/form words (sometimes combined with mild stuttering), weakness and visual disturbances such as lights seeming too bright, fuzzy or tunnel vision, black cloud-like spots in vision, and a feeling of nervousness can occur as well. The symptoms last for a few seconds before the loss of consciousness (if it is lost), which typically happens when the person is sitting up or standing.
When sufferers pass out, they fall down (unless prevented from doing so) and, when in this position, effective blood flow to the brain is immediately restored, allowing the person to regain consciousness. If the person does not fall into a fully flat, supine position, and the head remains elevated above the trunk, a state similar to a seizure may result from the blood's inability to return quickly to the brain, and the neurons in the body will fire off and generally cause muscles to twitch very slightly but mostly remain very tense. Fainting occurs with a loss of oxygen to the brain.
The autonomic nervous system's physiological state (see below) leading to loss of consciousness may persist for several minutes, so
Cause
Vasovagal syncope occurs in response to a trigger, with a corresponding malfunction in the parts of the nervous system that regulate heart rate and blood pressure. When heart rate slows, blood pressure drops, and the resulting lack of blood to the brain causes fainting and confusion.
Typical triggers for vasovagal episodes include:
Pathophysiology
Regardless of the trigger, the mechanism of syncope is similar in the various vasovagal syncope syndromes. The nucleus tractus solitarii of the brainstem is activated directly or indirectly by the triggering stimulus, resulting in simultaneous enhancement of parasympathetic nervous system (vagal) tone and withdrawal of sympathetic nervous system tone.
This results in a spectrum of hemodynamic responses:
- On one end of the spectrum is the cardioinhibitory response, characterized by a drop in heart rate (negative chronotropic effect) and in contractility (negative inotropic effect) leading to a decrease in cardiac output that is significant enough to result in a loss of consciousness. It is thought that this response results primarily from enhancement in parasympathetic tone.
- On the other end of the spectrum is the vasodepressor response, caused by a drop in blood pressure (to as low as 80/20) without much change in heart rate. This phenomenon occurs due to vasodilation, probably as a result of withdrawal of sympathetic nervous system tone.
- The majority of people with vasovagal syncope have a mixed response somewhere between these two ends of the spectrum.
One account for these physiological responses is the Bezold-Jarisch reflex.
Diagnosis
In addition to the mechanism described above, a number of other medical conditions may cause syncope. Making the correct diagnosis for loss of consciousness is one of the most difficult challenges that a physician can face. The core of the diagnosis of vasovagal syncope rests upon a clear description by the patient of a typical pattern of triggers, symptoms, and time course. It is also pertinent to differentiate lightheadedness, seizures, vertigo, and hypoglycemia as other causes.
In patients with recurrent vasovagal syncope, diagnostic accuracy can often be improved with one of the following diagnostic tests:
- A tilt table test (results should be interpreted in the context of patients' clinical presentations and with an understanding of the sensitivity and specificity of the test)
- Implantation of an insertable loop recorder
- A Holter monitor or event monitor
- An echocardiogram
- An electrophysiology study
Treatment
Treatment for vasovagal syncope focuses on avoidance of triggers, restoring blood flow to the brain during an impending episode, and measures that interrupt or prevent the pathophysiologic mechanism described above.
Prognosis
Brief periods of unconsciousness do no harm and are seldom symptoms of disease.
The main danger of vasovagal syncope (or dizzy spells from vertigo) is the risk of injury by falling while unconscious. Medication therapy could possibly prevent future vasovagal responses; however, for some individuals medication is ineffective and they will continue to have fainting episodes.
