Dorlands/Elsevier 12300668 | ||
 | ||
Latin Discus articularis articulationis radioulnaris distalis MeSH A02.835.583.405.930.800 | ||
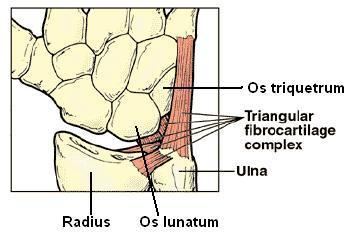
The Triangular fibrocartilage complex (TFCC) is formed by the triangular fibrocartilage discus (TFC), the radioulnar ligaments (RUL’s) and the ulnocarpal ligaments (UCL’s).
Contents
Structure
[[Gray336.png|thumb|Vertical section through the articulations at the wrist, showing the synovial cavities. (Articular disc labeled at center right.)]]
Triangular fibrocartilage disc
The TFC is an articular discus that lies on the pole of the distal ulna. It has a triangular shape and a biconcave body; the periphery is thicker than its center. The central portion of the TFC is thin and consists of chondroid fibrocartilage; this type of tissue is often seen in structures that can bear compressive loads. This central area is often so thin that it is translucent and in some cases it is even absent. The peripheral portion of the TFC is well vascularised, while the central portion has no blood supply.
This discus is attached by thick tissue to the base of the ulnar styloid and by thinner tissue to the edge of the radius just proximal to the radiocarpal articular surface.
Radioulnar ligaments
The RUL’s are the principal stabilizers of the distal radioulnar joint (DRUJ). There are two RUL's, the palmar and dorsal radioulnar ligaments.
These ligaments arise from the distal radius medial border and insert on the ulna at two separate and distinct sites: the ulna styloid and the fovea (a groove that separates the ulnar styloid from the ulnar head). Each ligament consists of a superficial component and a deep component. The superficial components insert directly onto the ulna styloid. The deep components insert more lateral, into the fovea adjacent to the articular surface of the pole of the distal ulna.
The ligaments are composed of longitudinally oriented lamellar collagen to resist tensile loads and have a rich vascular supply to allow healing.
Ulnocarpal ligaments
The UCL’s consist of the ulnolunate and the ulnotriquetral ligaments. They originate from the ulnar styloid and insert into the carpal bones of the wrist: the ulnolunate ligament inserts into the lunate bone and the ulnotriquetral ligament into the triquetrum bone. These ligaments prevent dorsal migration of the distal ulna. They are more taut during supination, because in supination ulnar styloid moves away from the carpal bones volar side.
Function
The primary functions of the TFCC:
Load transmission
The TFCC is important in load transmission across the ulnar aspect of the wrist. The TFC transmits and absorbs compressive forces.
The ulnar variance influences the amount of load that is transmitted through the distal ulna. The load transmission is directly proportional to this ulnar variance. In neutral ulnar variance, approximately 20 percent of the load is transmitted. With negative ulnar variance, the load across the TFC is decreased. This occurs during supination, because the radius moves distally on the ulna and creates a negative ulnar variance. With positive ulnar variance it is reversed. The load that is transmitted across the TFC is then increased. This positive ulnar variance occurs during pronation.
Rotation
The TFCC is a major stabilizer of the DRUJ. To control the forearm rotation the DRUJ acts in concert with the proximal radioulnar joint. The connection between the distal radius and the distal ulna, maintain the congruency of the DRUJ. This attachment is mainly created by the RUL’s of the TFCC. These ligaments support the joint through its arc of rotation.
The role of the TFCC in supination and in pronation is a matter of dispute. Some authors (Schuind et al.) concluded that the dorsal fibers of the TFCC tighten in pronation, and the palmar fibers in supination. These conclusions are opposite of those published by Af Ekenstam and Hagert.
Both parties are in fact right, because the RUL’s such as described in the anatomy, consist of two ligaments and each ligament has 2 components: the superficial and the deep ligament. During supination the superficial palmar and the deep dorsal ligaments are tighten, they prevent palmar translation of the ulna. In pronation this is reversed, the superficial dorsal and the deep palmar ligaments are tighten. They prevent dorsal translation of the ulna in pronation.
Clinical significance
The TFCC has a substantial risk for injury and degeneration because of its anatomic complexity and multiple functions.
Application of an extension-pronation force to an axial-load wrist, such as in a fall on an outstretched hand, causes most of the traumatic injuries of the TFCC.
Dorsal rotation injury, such as when a drill binds and rotates the wrist instead of the bit, can also cause traumatic injuries.
Injury may also occur from a distraction force applied to the volar forearm or wrist. Finally tears of the TFCC are frequently found by patients with distal radius fractures.
Perforations and defects in the TFCC are not all traumatic. There is an age related correlation with lesions in the TFCC, but many of these defects are asymptomatic. These lesions common occur by patients with positive ulnar variance.
Chronic and excessive loading through the ulnocarpal joint, causes degenerative TFCC tears. These tears are a component of ulnar impaction syndrome.
Even though natural degeneration of the ulnocarpal joint is very common, it is important to recognize. In cadavaric examinations, 30% to 70% of the cases had TFCC perforations and chondromalacia of the ulnar head, lunate and triquetrum. Cases with ulnar-negative variance had fewer degenerative changes.
Palmer’s classifications of TFCC Lesions
The Palmer classification is the most recognized scheme; it divides TFCC lesions into these two categories. This classification provides an accurate anatomic description of tears, it does not guide treatment or indicate prognosis.
Symptoms
Patients with a TFCC injury usually experience pain or discomfort located at the ulnar side of the wrist, often just above the ulnar styloid. However, there are also some patients who report diffuse pain throughout the entire wrist.
Rest can reduce pain and activity can make it worse, especially with rotating movements (supination and pronation) of the wrist or movements of the hand sideways in ulnar direction.
Other symptoms patients with a TFCC injury frequently mention are: swelling, loss of grip strength, instability and grinding or clicking sounds (crepitus) that can occur during activity of the wrist.
Diagnosis
Injuries to the TFCC may be preceded by a fall on a pronated outstretched arm; a rotational injury to the forearm; an axial load trauma to the wrist; or a distraction injury of the wrist in ulnar direction. However, not all patients can recall a preceding trauma occurred.
Imaging
Note: Imaging techniques can only be relevant together with the clinical findings of a carefully performed physical examination.
Other than a TFCC injury, there are many possible causes for ulnar-sided wrist pain.
Differentiate diagnosis of TFCC injuries
Treatment
The initial treatment for both traumatic and degenerative TFCC lesions, with a stable DRUJ, is conservative (nonsurgical) therapy. Patients may be advised to wear a temporary splint or cast to immobilize the wrist and forearm for four to six weeks. The immobilization allows scar tissue to develop which can help heal the TFCC. In addition oral NSAID’s and corticosteroid joint injections can be prescribed for pain relief. Physiotherapy and Occupational Therapy can help patients recover after immobilization or surgery. Wrist support straps used in sports can also be used in mild cases to compress and minimize movement of the area.
Indications for acute TFCC surgery are: a clearly unstable DRUJ, or the existence of additional unstable or displaced fractures. TFCC surgery is also indicated when conservative treatment proves insufficient in about 8–12 weeks.
Fractures of the radius bone are often associated by TFCC damage. If the fracture is treated surgically it is recommended to evaluate and if necessary repair the TFCC as well. Closed fractures (where the skin is still intact) of the radius bone are treated non-surgically with cast; the immobilization can also help heal the TFCC.
Surgical
The central part of the TFC has no blood supply and therefore has no healing capacity. When a tear occurs in this area of the TFC, it typically creates an unstable flap of tissue that is likely to catch on other joint surfaces. Removing the damaged tissue (debridement) is then indicated. Arthroscopic debridement as a treatment for degenerative TFC tears associated with positive ulnar variance, unfortunately, show poor results.
Suturing TFCC ligaments can sometimes be performed arthroscopically. But only if there is no serious damage to the ligaments or other surrounding structures. Even after a short period of time torn ligaments tend to retract and therefore lose length. Retracted ligament ends are impossible to suture together again and a reconstruction may be necessary.
Open surgery is usually required for degenerative or more complex TFCC injuries, or if additional damage to the wrist or forearm caused instability or displacement. It is a more invasive surgical technique compared to arthroscopic treatment, but the surgeon has better visibility and access to the TFCC.
