Trade names Exelon MedlinePlus a602009 Molar mass 250.337 g/mol Protein binding 40% | AHFS/Drugs.com Monograph ATC code N06DA03 (WHO) CAS ID 123441-03-2 | |
 | ||
Pregnancycategory US: B (No risk in non-human studies) Routes ofadministration Oral, transdermal patch | ||
Exelon patch rivastigmine patch for alzheimer s
Rivastigmine (sold under the trade name Exelon) is a parasympathomimetic or cholinergic agent for the treatment of mild to moderate dementia of the Alzheimer's type and dementia due to Parkinson's disease. The drug can be administered orally or via a transdermal patch; the latter form reduces the prevalence of side effects, which typically include nausea and vomiting.
Contents
- Exelon patch rivastigmine patch for alzheimer s
- Medical uses
- Efficacy
- Side effects
- Administration
- Pharmacodynamics
- Pharmacokinetics
- History
- References
The drug is eliminated through the urine, and appears to have relatively few drug-drug interactions.
Medical uses
Rivastigmine capsules, liquid solution and patches are used for the treatment of mild to moderate dementia of the Alzheimer's type and for mild to moderate dementia related to Parkinson's disease.
Rivastigmine has demonstrated treatment effects on the cognitive (thinking and memory), functional (activities of daily living) and behavioural problems commonly associated with Alzheimer's and Parkinson's disease dementias.
Efficacy
In people with either type of dementia, rivastigmine has been shown to provide meaningful symptomatic effects that may allow patients to remain independent and ‘be themselves’ for longer. In particular, it appears to show marked treatment effects in patients showing a more aggressive course of disease, such as those with younger onset ages, poor nutritional status, or those experiencing symptoms such as delusions or hallucinations. For example, the presence of hallucinations appears to be a predictor of especially strong responses to rivastigmine, both in Alzheimer's and Parkinson's patients. These effects might reflect the additional inhibition of butyrylcholinesterase, which is implicated in symptom progression and might provide added benefits over acetylcholinesterase-selective drugs in some patients. Multiple-infarct dementia patients may show slight improvement in executive functions and behaviour. No firm evidence supports usage in schizophrenia patients.
Its efficacy is similar to donepezil and tacrine. Doses below 6 mg/d may be ineffective. The effects of this kind of drug in different kinds of dementia (including Alzheimer's dementia) are modest, and it is still unclear which AcCh(ButCh) esterase inhibitor is better in Parkinson's dementia, though rivastigmine is well-studied.
Side effects
Side effects may include nausea and vomiting, decreased appetite and weight loss.
The strong potency of rivastigmine, provided by its dual inhibitory mechanism, has been postulated to lead to more nausea and vomiting during the titration phase of oral rivastigmine treatment. This enforces the importance of taking oral forms of these drugs with food as prescribed. However, rates of nausea and vomiting are markedly reduced with the once-daily rivastigmine patch (which can be applied at any time of the day, with or without food). Patients and caregivers should be aware of warning signs of potential toxicities and know when to call their doctor. For the patch and oral formulations, skin rashes can occur at which time patients should contact their doctor immediately. For the patch, patients and caregivers should monitor for any intense itching, redness, swelling or blistering at the patch location. If this occurs, remove the patch, rinse the area and call the doctor immediately.
In a large clinical trial of the rivastigmine patch in 1,195 patients with Alzheimer's disease, the target dose of 9.5 mg/24-hour patch provided similar clinical effects (e.g. memory and thinking, activities of daily living, concentration) as the highest doses of rivastigmine capsules, but with one-third fewer reports of nausea and vomiting.
Usage of rivastigmine was associated with a higher frequency of reports of death as an adverse event in the Food and Drug Administration Adverse Event Reporting System database compared to the other acetylcholinesterase inhibiting drugs donepezil and galantamine.
Administration
Rivastigmine tartrate is a white to off-white, fine crystalline powder that is both lipophilic (soluble in fats) and hydrophilic (soluble in water). It comes in a variety of administrations including a capsule, solution and a transdermal patch. Like other cholinesterase inhibitors, it requires doses to be increased gradually over several weeks; this is usually referred to as the titration phase. Oral doses of rivastigmine should be titrated with a 3 mg per day increment every 2 to 4 weeks. For oral dosing, an initial dose of 1.5 mg twice daily is recommended followed by an increase by 1.5 mg/dose after four weeks. The dose should increase as long as side effects are tolerable. Patients should be reminded to take with food. For the transdermal patch, an initial dose of 4.6 mg per day increases to 9.5 mg per day after four weeks if the patient is not experiencing any intolerable side effects. Patients or caregivers should be reminded to remove the old patch every day, rotate sites and place a new one. It is recommended that the patch be applied to the upper back or torso.
Rivastigmine is classified as pregnancy category B, with insufficient data on risks associated with breastfeeding. In cases of overdose, atropine is used to reverse bradycardia. Dialysis is ineffective due to the drug's half-life.
Pharmacodynamics
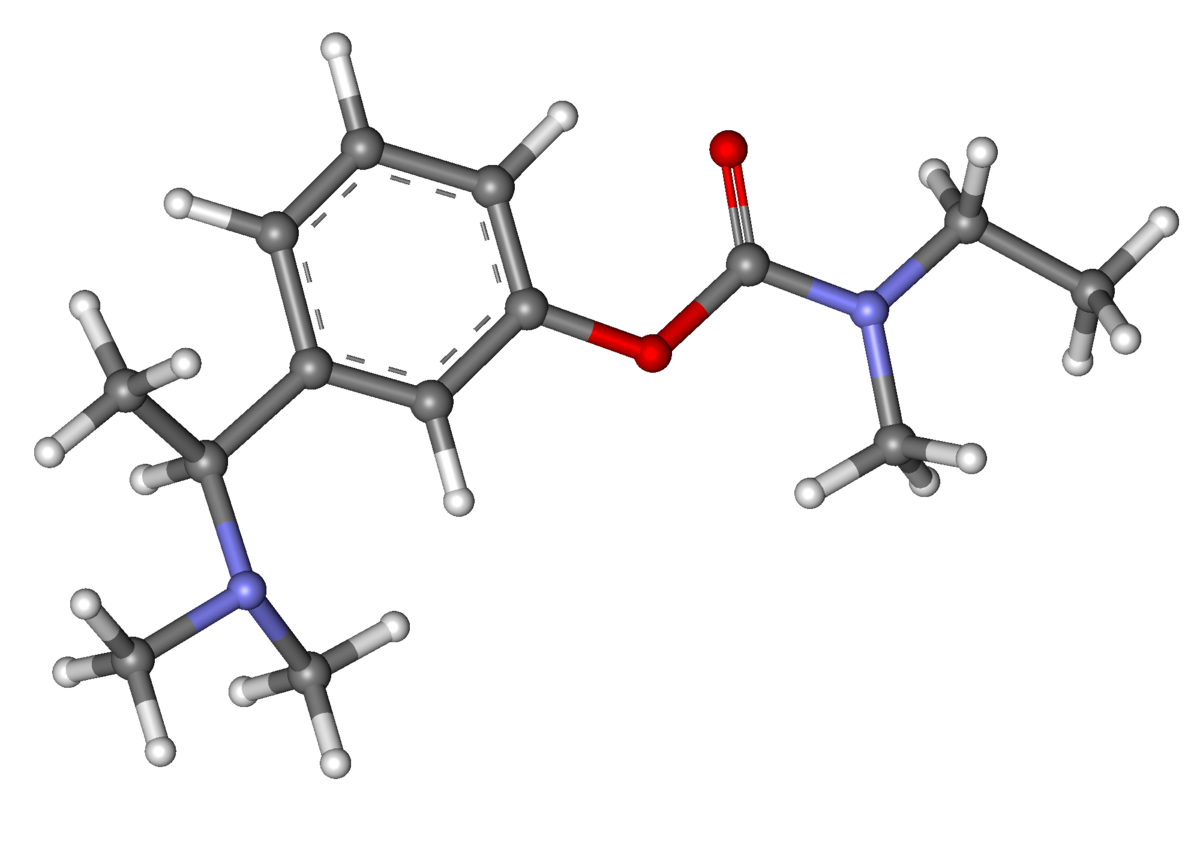
Rivastigmine, an acetylcholinesterase inhibitor, inhibits both butyrylcholinesterase and acetylcholinesterase (unlike donepezil, which selectively inhibits acetylcholinesterase). It is thought to work by inhibiting these cholinesterase enzymes, which would otherwise break down the brain neurotransmitter acetylcholine.
Pharmacokinetics
When given orally, rivastigmine is well absorbed, with a bioavailability of about 40% in the 3-mg dose. Pharmacokinetics are linear up to 3 mg BID, but nonlinear at higher doses. Elimination is through the urine. Peak plasma concentrations are seen in about one hour, with peak cerebrospinal fluid concentrations at 1.4–3.8 hours. When given by once-daily transdermal patch, the pharmacokinetic profile of rivastigmine is much smoother, compared with capsules, with lower peak plasma concentrations and reduced fluctuations. The 9.5 mg/24 h rivastigmine patch provides comparable exposure to 12 mg/day capsules (the highest recommended oral dose).
The compound does cross the blood–brain barrier. Plasma protein binding is 40%. The major route of metabolism is by its target enzymes via cholinesterase-mediated hydrolysis. Elimination bypasses the hepatic system, so hepatic cytochrome P450 (CYP) isoenzymes are not involved. The low potential for drug-drug interactions (which could lead to adverse effects) has been suggested as due to this pathway compared to the many common drugs that use the cytochrome P450 metabolic pathway.
History
Rivastigmine was developed by Marta Weinstock-Rosin of the Department of Pharmacology at the Hebrew University of Jerusalem and sold to Novartis by Yissum for commercial development. It is a semi-synthetic derivative of physostigmine. It has been available in capsule and liquid formulations since 1997. In 2006, it became the first product approved globally for the treatment of mild to moderate dementia associated with Parkinson's disease; and in 2007 the rivastigmine transdermal patch became the first patch treatment for dementia.
