Specialty rheumatology ICD-9-CM 446.0 MedlinePlus 001438 | ICD-10 M30.0 DiseasesDB 10220 MeSH D010488 | |
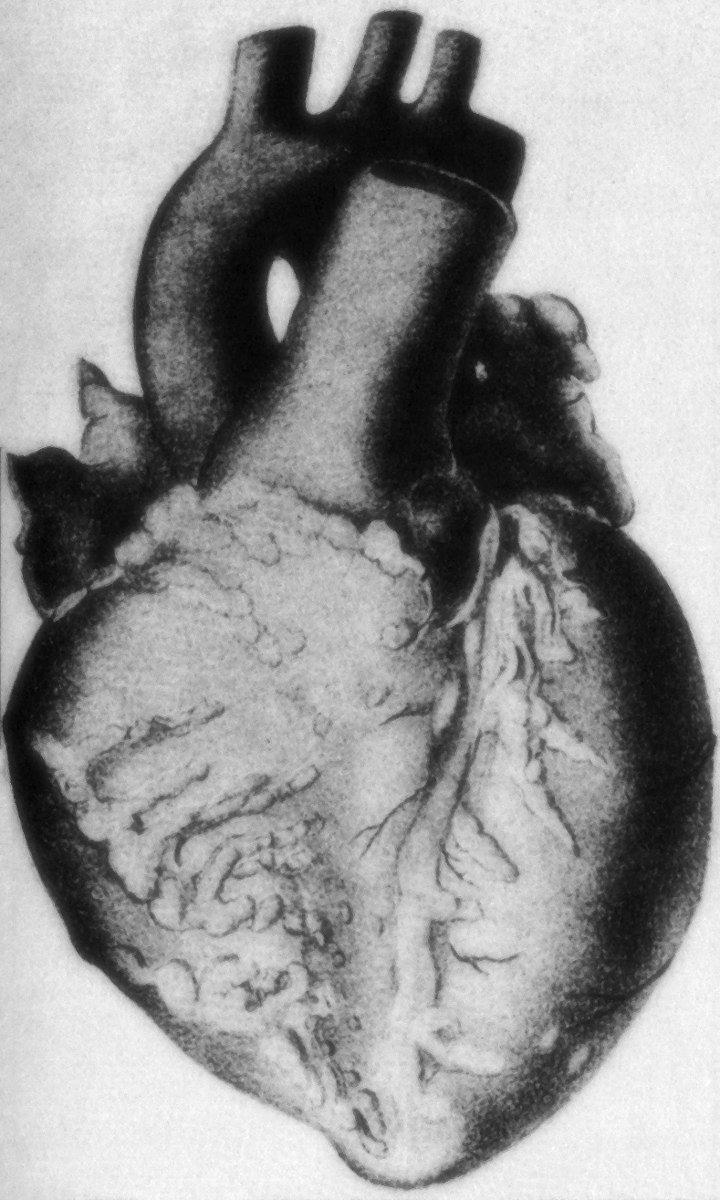 | ||
Polyarteritis nodosa, also known as panarteritis nodosa, periarteritis nodosa, Kussmaul disease, Kussmaul-Maier disease or PAN, is a systemic vasculitis of small- or medium-sized muscular arteries, typically involving renal and visceral vessels but sparing the pulmonary circulation. Polyarteritis nodosa may present in infants. In polyarteritis nodosa, small aneurysms are strung like the beads of a rosary, therefore making "rosary sign" an important diagnostic feature of the vasculitis.
Contents
With treatment, five-year survival is 80%; without treatment, five-year survival is 13%. Death is often a consequence of kidney failure, myocardial infarction, or stroke.
Signs and symptoms
In this disease, symptoms result from ischemic damage to affected organs, often the skin, heart, kidneys, and nervous system. Generalised symptoms include fever, fatigue, weakness, loss of appetite, and weight loss. Muscle and joint aches are common. The skin may show rashes, swelling, ulcers, and lumps. Palpable purpura and livedo reticularis can occur in some patients.
Nerve involvement may cause sensory changes with numbness, pain, burning, and weakness (peripheral neuropathy). Central nervous system involvement may cause strokes or seizures. Kidney involvement can produce varying degrees of kidney failure, such as hypertension, edema, oliguria, and uremia. Involvement of the arteries of the heart may cause a heart attack, heart failure, and inflammation of the sac around the heart (pericarditis).
Causes
There is no association with ANCA, but about 30% of patients with PAN have chronic hepatitis B and deposits containing HBsAg-HBsAb complexes in affected vessels, indicating an immune complex–mediated etiology in that subset. The cause remains unknown in the remaining cases; there may be etiologic and clinical distinctions between classic idiopathic PAN, the cutaneous forms of PAN, and the PAN associated with chronic hepatitis.
Diagnosis
No specific lab tests exist for diagnosing polyarteritis nodosa. Diagnosis is generally based on the physical examination and a few laboratory studies that help confirm the diagnosis:
A patient is said to have polyarteritis nodosa if he or she has three of the 10 signs known as the 1990 American College of Rheumatology (ACR) criteria, when a radiographic or pathological diagnosis of vasculitis is made:
In polyarteritis nodosa, small aneurysms are strung like the beads of a rosary, therefore making "rosary sign" an important diagnostic feature of the vasculitis. The 1990 ACR criteria were designed for classification purposes only. Nevertheless, their good discriminatory performances, indicated by the initial ACR analysis, suggested their potential usefulness for diagnostic purposes as well. Subsequent studies did not confirm their diagnostic utility, demonstrating a significant dependence of their discriminative abilities on the prevalence of the various vasculitides in the analyzed populations. Recently, an original study, combining the analysis of more than 100 items used to describe patients' characteristics in a large sample of vasculitides with a computer simulation technique designed to test the potential diagnostic utility of the various criteria, proposed a set of eight positively or negatively discriminating items to be used as a screening tool for diagnosis in patients suspected of systemic vasculitis.
Treatment
Treatment involves medications to suppress the immune system, including prednisone and cyclophosphamide. In some cases, methotrexate or leflunomide may be helpful. Some patients have also noticed a remission phase when a four-dose infusion of rituximab is used before the leflunomide treatment is begun. Therapy results in remissions or cures in 90% of cases. Untreated, the disease is fatal in most cases. The most serious associated conditions generally involve the kidneys and gastrointestinal tract. A fatal course usually involves gastrointestinal bleeding, infection, myocardial infarction, and/or kidney failure.
In case of remission, about 60% experience relapse within five years. In cases caused by hepatitis B virus, however, recurrence rate is only around 6%.
Epidemiology
The condition affects adults more frequently than children and males more frequently than females. Most cases occur between the ages of 30 and 49. It damages the tissues supplied by the affected arteries because they do not receive enough oxygen and nourishment without a proper blood supply. Polyarteritis nodosa is more common in people with hepatitis B infection.
In popular media
The 1956 film Bigger Than Life featured the protagonist being diagnosed with polyarteritis nodosa.
