Specialty Obstetrics ICD-9-CM 641.0, 641.1 MeSH D010923 | ICD-10 O44, P02.0 MedlinePlus 000900 | |
 | ||
Placenta previa is an obstetric complication in which the placenta is inserted partially or wholly in the lower uterine segment. It is a leading cause of antepartum haemorrhage (vaginal bleeding). It affects approximately 0.4-0.5% of all labours.
Contents
- Signs and symptoms
- Cause
- Classification
- Risk factors
- Diagnosis
- Confirmatory
- Management
- Mode of delivery
- Maternal
- Fetal
- Epidemiology
- History
- References
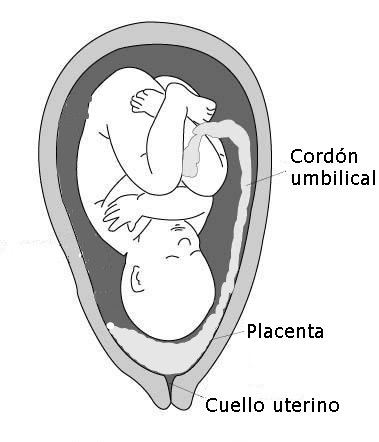
In the last trimester of pregnancy the isthmus of the uterus unfolds and forms the lower segment. In a typical pregnancy the placenta does not overlie. If the placenta does overlie the lower segment, as is the case with placenta previa, it may shear off and a small section may bleed.
Signs and symptoms
Women with placenta previa often present with painless, bright red vaginal bleeding. This commonly occurs around 32 weeks of gestation, but can be as early as late mid-trimester. This bleeding often starts mildly and may increase as the area of placental separation increases. Previa should be suspected if there is bleeding after 24 weeks of gestation.
Women may also present as a case of failure of engagement of fetal head.
Cause
Exact cause of placenta previa is unknown. It is hypothesized to be related to abnormal vascularisation of the endometrium caused by scarring or atrophy from previous trauma, surgery, or infection. These factors may reduce differential growth of lower segment, resulting in less upward shift in placental position as pregnancy advances.
Classification
Traditionally, four grades of placenta previa were used, however now it is more common to simply differentiate between 'major' and 'minor' cases.
Risk factors
The following have been identified as risk factors for placenta previa:
Placenta previa is itself a risk factor of placenta accreta.
Diagnosis
History may reveal antepartum hemorrhage. Abdominal examination usually finds the uterus non-tender, soft and relaxed. Leopold's Maneuvers may find the fetus in an oblique or breech position or lying transverse as a result of the abnormal position of the placenta. Malpresentation is found in about 35% cases. Vaginal examination is avoided in known cases of placenta previa.
Confirmatory
Previa can be confirmed with an ultrasound. Transvaginal ultrasound has superior accuracy as compared to transabdominal one, thus allowing measurement of distance between placenta and cervical os. This has rendered traditional classification of placenta previa obsolete.
False positives may be due to following reasons:
In such cases, repeat scanning is done after an interval of 15–30 minutes.
In parts of the world where ultrasound is unavailable, it is not uncommon to confirm the diagnosis with an examination in the surgical theatre. The proper timing of an examination in theatre is important. If the woman is not bleeding severely she can be managed non-operatively until the 36th week. By this time the baby's chance of survival is as good as at full term.
Management
An initial assessment to determine the status of the mother and fetus is required. Although mothers used to be treated in the hospital from the first bleeding episode until birth, it is now considered safe to treat placenta previa on an outpatient basis if the fetus is at less than 30 weeks of gestation, and neither the mother nor the fetus are in distress. Immediate delivery of the fetus may be indicated if the fetus is mature or if the fetus or mother are in distress. Blood volume replacement (to maintain blood pressure) and blood plasma replacement (to maintain fibrinogen levels) may be necessary.
The corticosteroids are indicated at 24–34 weeks gestation if the patient has bleeding, given the higher risk of premature birth. [Citation needed]
Mode of delivery
The mode of delivery is determined by clinical state of the mother, fetus and ultrasound findings. In minor degrees (traditional grade I and II), vaginal delivery is possible. RCOG recommends that the placenta should be at least 2 cm away from internal os for an attempted vaginal delivery. When a vaginal delivery is attempted, consultant obstetrician and anesthetists are present in delivery suite. In cases of fetal distress and major degrees (traditional grade III and IV) a caesarean section is indicated. Caesarian section is contraindicated in cases of disseminated intravascular coagulation. An obstetrician may need to divide the anterior lying placenta. In such cases, blood loss is expected to be high and thus blood and blood products are always kept ready. In rare cases, hysterectomy may be required. In the U.S., women with placenta previa who are covered by private insurance are 22% more likely to receive a caesarean section than women covered by Medicaid.
Maternal
Fetal
Epidemiology
Placenta previa occurs approximately one of every 250 births. One third of all antepartum hemorrhage occurs due to placenta previa. It has been suggested that incidence of placenta previa is increasing due to increased rate of Caesarian section.
Perinatal mortality rate of placenta previa is 3-4 times higher than normal pregnancies.
History
In places where a Caesarean section could not be performed due to the lack of a surgeon or equipment, infant could be delivered vaginally. There were two ways of doing this with a placenta previa:
