Specialty Cardiology ICD-9-CM 427.0 | ICD-10 I47.1 MeSH D013617 | |
 | ||
Synonyms supraventricular tachycardia, paroxysmal atrial tachycardia (PAT) | ||
Paroxysmal supraventricular tachycardia (PSVT) is a type of supraventricular tachycardia. Often people have no symptoms. Otherwise symptoms may include palpitations, feeling lightheaded, sweating, shortness of breath, and chest pain. Episodes start and end suddenly.
Contents
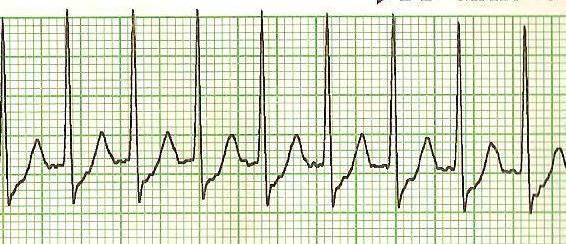
The cause is not known. Risk factors include alcohol, caffeine, nicotine, psychological stress, and Wolff-Parkinson-White syndrome which often is inherited from a person's parents. The underlying mechanism typically involves an accessory pathway that results in re-entry. Diagnosis is typically by an electrocardiogram (ECG) which shows narrow QRS complexes and a fast heart rhythm typically between 150 and 240 beats per minute.
Vagal maneuvers, such as the valsalva maneuver, are often used as the initial treatment. If not effective and the person has a normal blood pressure the medication adenosine may be tried. If adenosine is not effective a calcium channel blockers or beta blocker maybe used. Otherwise synchronized cardioversion is the treatment. Future episodes can be prevented by catheter ablation.
About 2.3 per 1000 people have paroxysmal supraventricular tachycardia. Problems typically begin in those 12 to 45 years old. Women are more often affected than men. Outcomes in those who otherwise have a normal heart are generally good. An ultrasound of the heart may be done to rule out underlying heart problems.
Signs and symptoms
Symptoms may include palpitations, feeling faint, sweating, shortness of breath, and chest pain. Episodes start and end suddenly.
Types
Treatment
AV nodal blocking can be achieved in at least three ways:
Physical maneuvers
A number of physical maneuvers increase the resistance of the AV node to transmit impulses (AV nodal block), principally through activation of the parasympathetic nervous system, conducted to the heart by the vagus nerve. These manipulations are collectively referred to as vagal maneuvers.
The valsalva maneuver should be the first vagal maneuver tried and works by increasing intra-thoracic pressure and affecting baroreceptors (pressure sensors) within the arch of the aorta. It is carried out by asking the patient to hold his/her breath while trying to exhale forcibly as if straining during a bowel movement. Holding the nose and exhaling against the obstruction has a similar effect.
There are other vagal maneuvers including: holding one's breath for a few seconds, coughing, plunging the face into cold water, (via the diving reflex), drinking a glass of ice cold water, and standing on one's head. Carotid sinus massage, carried out by firmly pressing the bulb at the top of one of the carotid arteries in the neck, is effective but is often not recommended in the elderly due to the potential risk of stroke in those with atherosclerotic plaque in the carotid arteries.
Pressing down gently on the top of closed eyes may also bring heartbeat back to normal rhythm for some people with atrial or supraventricular tachycardia (SVT).
Medications
Adenosine, an ultra-short-acting AV nodal blocking agent, is indicated if vagal maneuvers are not effective. If unsuccessful or the PSVT recurs diltiazem or verapamil are recommended. Adenosine may be safely used during pregnancy.
SVT that does not involve the AV node may respond to other anti-arrhythmic drugs such as sotalol or amiodarone.
Cardioversion
If the person is hemodynamically unstable or other treatments have not been effective, synchronized electrical cardioversion may be used. In children this is often done with a dose of 0.5 to 1 J/Kg.
