Species Human Entrez 6331 | Human Mouse Ensembl ENSG00000183873 | |
 | ||
Aliases SCN5A, CDCD2, CMD1E, CMPD2, HB1, HB2, HBBD, HH1, ICCD, IVF, LQT3, Nav1.5, PFHB1, SSS1, VF1, sodium voltage-gated channel alpha subunit 5 External IDs OMIM: 600163 MGI: 98251 HomoloGene: 22738 GeneCards: SCN5A | ||
NaV1.5 is an integral membrane protein and tetrodotoxin-resistant voltage-gated sodium channel subunit. NaV1.5 is found primarily in cardiac muscle, where it mediates the fast influx of Na+-ions (INa) across the cell membrane, resulting in the fast depolarization phase of the cardiac action potential. As such, it plays a major role in impulse propagation through the heart. A vast number of cardiac diseases is associated with mutations in NaV1.5 (see paragraph genetics). SCN5A is the gene that encodes the cardiac sodium channel NaV1.5.
Contents
Gene structure
SCN5A is a highly conserved gene located on human chromosome 3, where it spans more than 100 kb. The gene consists of 28 exons, of which exon 1 and in part exon 2 form the 5’ untranslated region (5’UTR) and exon 28 the 3’ untranslated region (3’UTR) of the RNA. SCN5A is part of a family of 10 genes that encode different types of sodium channels, i.e. brain-type (NaV1.1, NaV1.2, NaV1.3, NaV1.6), neuronal channels (NaV1.7, NaV1.8 and NaV1.9), skeletal muscle channels (NaV1.4) and the cardiac sodium channel NaV1.5.
Expression pattern
SCN5A is mainly expressed in the heart, where expression is abundant in working myocardium and conduction tissue. In contrast, expression is low in the sinoatrial node and atrioventricular node. Within the heart, a transmural expression gradient from subendocardium to subsendocardium is present, with higher expression of SCN5A in the endocardium as compared to the epicardium
Splice variants
More than 10 different splice isoforms have been described for SCN5A, of which several harbour different functional properties. In the heart, two isoforms are mainly expressed (ratio 1:2), of which the least predominant one contains an extra glutamine at position 1077 (1077Q). Moreover, different isoforms are expressed during fetal life and adult, differing in the inclusion of an alternative exon 6.
Protein structure and function
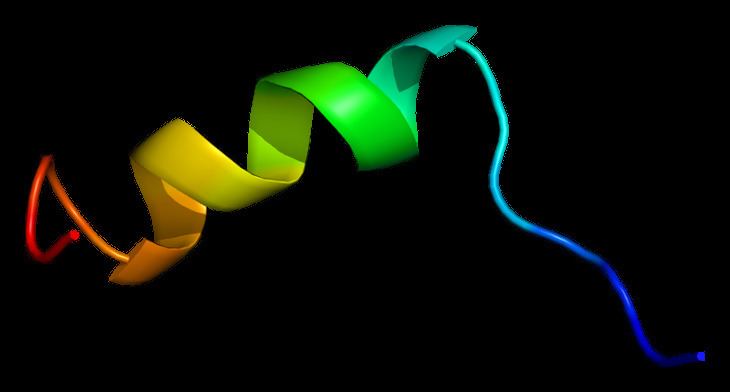
NaV1.5 is a large transmembrane protein with 4 repetitive transmembrane domains (DI-DIV), containing 6 transmembrane spanning sections each (S1-S6). The pore region of the channels, through which Na+-ions flow, are formed by the segments S5 and S6 of the 4 domains. Voltage sensing is mediated by the remaining segments, of which the positively charged S4 segments plays a fundamental role.
NaV1.5 channels predominantly mediate the sodium current (INa) in cardiac cells. INa is responsible for the fast upstroke of the action potential, and as such plays a crucial role in impulse propagation through the heart. The conformational state of the channel, which is both voltage and time-dependent, determines whether the channel is opened or closed. At the resting membrane potential (around -85 mV), NaV1.5 channels are closed. Upon a stimulus (through conduction by a neighboring cell), the membrane depolarizes and NaV1.5 channels open through the outward movement of the S4 segments, leading to the initiation of the action potential. Simultaneously, a process called ‘fast inactivation’ results in closure of the channels within 1 ms. In physiological conditions, when inactivated, channels remain in closed state until the cell membrane repolarizes, where a recovery from inactivation is necessary before they become available for activation again. During the action potential, a very small fraction of sodium current persists and does not inactivate completely. This current is called ‘sustained current’, ‘late current’ or ‘INa,L’. Also, some channels may reactivate during the repolarizing phase of the action potential at a range of potentials where inactivation is not complete and shows overlap with activation, generating the so-called “window current”.
Sub-units and protein interaction partners
Trafficking, function and structure of NaV1.5 can be affected by the many protein interaction partners that have been identified to date (for an extensive review, see Abriel et al. 2010). Of these, the 4 sodium channel beta-subunits, encoded by the genes SCN1B, SCN2B, SCN3B and SCN4B, form an important category. In general, beta-subunits increase function of NaV1.5, either by change in intrinsic properties or by affecting the process of trafficking to the cell surface.
Apart from the beta-subunits, other proteins, such as calmodulin, calmodulin kinase II δc, ankyrin-G and plakophilin-2, are known to interact and modulate function of NaV1.5. Some of these have also been linked to genetic and acquired cardiac diseases.
Genetics
Mutations in SCN5A, which could result in a loss and/or a gain-of-function of the channel, are associated with a spectrum of cardiac diseases. Pathogenic mutations generally exhibit an autosomal dominant inheritance pattern, although recessive forms of SCN5A mutations are also described. Also, mutations may act as a disease modifier, especially in families where lack of direct causality is reflected by complex inheritance patterns. It is important to note that a significant amount of individuals (2-7%) in the general population carry a rare (population frequency <1%), protein-altering variant in the gene, highlighting the complexity of linking mutations directly with observed phenotypes. Mutations that result in the same biophysical effect can give rise to different diseases.
To date, loss-of-function mutations have been associated with Brugada syndrome (BrS), progressive cardiac conduction disease (Lev-Lenègre disease), dilated cardiomyopathy (DCM), sick sinus syndrome, and atrial fibrillation.
Mutations resulting in a gain-of-function are causal for Long QT syndrome type 3 and are also more recently implicated in multifocal ectopic Purkinje-related premature contractions (MEPPC) Some gain-of-function mutations are also associated with AF and DCM. Gain-of-function of NaV1.5 is generally reflected by an increase in INa,L, a slowed rate of inactivation or a shift in voltage dependence of activation or inactivation (resulting in an increased window-current).
SCN5A variations in the general population
Genetic variations in SCN5A, i.e. single nucleotide polymorphisms (SNPs) have been described in both coding and non-coding regions of the gene. These variations are typically present at relatively high frequencies within the general population. Genome Wide Association Studies (GWAS) have used this type of common genetic variation to identify genetic loci associated with variability in phenotypic traits. In the cardiovascular field this powerful technique has been used to detect loci involved in variation in electrocardiographic parameters (i.e. PR-, QRS- and QTc-interval duration) in the general population. The rationale behind this technique is that common genetic variation present in the general population can influence cardiac conduction in non-diseased individuals. these studies consistently identified the SCN5A-SCN10A genomic region on chromosome 3 to be associated with variation in QTc-interval, QRS duration and PR-interval. These results indicate that genetic variation at the SCN5A locus is not only involved in disease #genetics but also plays a role in the variation in cardiac function between individuals in the general population.
NaV1.5 as a pharmacological target
The cardiac sodium channel NaV1.5 has since long been a common target in the pharmacologic treatment of arrhythmic events. Classically, sodium channel blockers that block the peak sodium current are classified as Class I anti-arrhythmic agents and further subdivided in class IA, IB and IC, depending on their ability to change the length of the cardiac action potential. Use of such sodium channel blockers is among others indicated in patients with ventricular reentrant tachyarrhythmia in the setting of cardiac ischemia and in patients with atrial fibrillation in absence of structural heart disease.
