Synonyms plural comedones ICD-9-CM 706.1 | ||
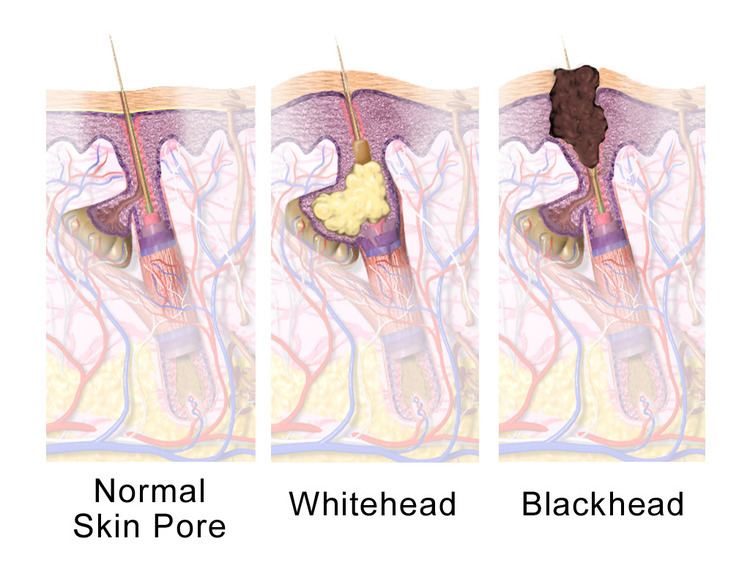 | ||
A comedo is a clogged hair follicle (pore) in the skin. Keratin (skin debris) combines with oil to block the follicle. A comedo can be open (blackhead) or closed by skin (whitehead), and occur with or without acne. The word comedo comes from the Latin comedere, meaning "to eat up", and was historically used to describe parasitic worms; in modern medical terminology, it is used to suggest the worm-like appearance of the expressed material.
Contents
The chronic inflammatory condition that usually includes both comedones and inflamed papules and pustules (pimples) is called acne. Infection causes inflammation and the development of pus. Whether or not a skin condition classifies as acne depends on the amount of comedones and infection. Comedones should not be confused with sebaceous filaments.
Comedo-type ductal carcinoma in situ (DCIS) is not related to the skin conditions discussed here. DCIS is a non-invasive form of breast cancer, but comedo-type DCIS may be more aggressive and so may be more likely to become invasive.
Causes
Oil production in the sebaceous glands increases during puberty, causing comedones and acne to be common in teenagers. Acne is also found pre-menstrually and in women with polycystic ovarian syndrome. Smoking may worsen acne.
Oxidation rather than poor hygiene or dirt causes blackheads to be black. Washing or scrubbing the skin too much could make it worse, by irritating the skin. Touching and picking at comedones might cause irritation and spread infection. It is not clear what effect shaving has on the development of comedones or acne.
Some, but not all, skin products might increase comedones by blocking pores, and greasy hair products (like pomades) can worsen acne. Skin products that claim to not clog pores may be labeled noncomedogenic or non-acnegenic. Make-up and skin products that are oil-free and water-based may be less likely to cause acne. It is not known whether dietary factors or sun exposure make comedones better, worse or have no effect.
A hair that does not emerge normally can also block the pore and cause a bulge or lead to infection (causing inflammation and pus).
Genes may play a role in the chances of developing acne. Comedones may be more common in some ethnic groups. People of African descent may experience more inflammation in comedones, more comedonal acne, and earlier onset of inflammation.
Pathophysiology
Comedones are associated with the pilosebaceous unit, which includes a hair follicle and sebaceous gland. These units are mostly on the face, neck, upper chest, shoulders and back. Excess keratin combined with sebum can plug the opening of the follicle. This small plug is called a microcomedo. Androgens increase sebum (oil) production. If sebum continues to build up behind the plug, it can enlarge and form a visible comedo.
A comedo may be open to the air ("blackhead") or closed by skin ("whitehead"). Being open to the air causes oxidization, which turns it black. Propionibacterium acnes is the suspected infectious agent in acne. It can proliferate in sebum and cause inflamed pustules (pimples) characteristic of acne. Nodules are inflamed, painful deep bumps under the skin.
Comedones that are 1 mm or larger are called macrocomedones. They are closed comedones and are more frequent on the face than neck.
Solar comedones (sometimes called senile comedones) are related to many years of exposure to the sun, usually on the cheeks, not to acne-related pathophysiology.
Management
Using non-oily cleansers and mild soap may not cause as much irritation to the skin as regular soap. Blackheads can be removed across an area with commercially available pore-cleansing strips or the more aggressive cyanoacrylate method used by dermatologists.
Squeezing blackheads and whiteheads can remove them, but it can also damage the skin. Doing so increases the risk of causing or transmitting infection and scarring, as well as potentially pushing any infection deeper into the skin. Comedo extractors are used with careful hygiene in beauty salons and by dermatologists, usually after using steam or warm water.
Complementary medicine options for acne in general have not been shown to be effective in trials. These include aloe vera, pyridoxine (vitamin B6), fruit-derived acids, kampo (Japanese herbal medicine), ayurvedic herbal treatments and acupuncture.
Some acne treatments target infection specifically, but there are treatments that are aimed at the formation of comedones as well. Others remove the dead layers of the skin and may help clear blocked pores.
Dermatologists can often extract open comedones with minimal skin trauma, but closed comedones are more difficult. Laser treatment for acne might reduce comedones, but dermabrasion and laser therapy have also been known to cause scarring.
Macrocomedones (1 mm or larger) can be removed by a dermatologist using surgical instruments or cauterized with a device that uses light. The acne drug isotretinoin can cause severe flare-ups of macrocomedones, so dermatologists recommend removal before starting the drug and during treatment.
Some research suggests that the common acne medications, retinoids and azelaic acid, are beneficial and do not cause increased pigmentation of the skin.
Rare conditions
Favre–Racouchot syndrome occurs in sun-damaged skin and includes open and closed comedones.
Nevus comedonicus or comedo nevus is a benign hamartoma (birthmark) of the pilosebaceous unit around the oil-producing gland in the skin. It has widened open hair follicles with dark keratin plugs that resemble comedones, but they are not actually comedones.
Dowling-Degos disease is a genetic pigment disorder that includes comedo-like lesions and scars.
Familial dyskeratotic comedones is a rare autosomal dominant genetic condition, with keratotic (tough) papules and comedo-like lesions.
