ICD-9-CM 348.82 MeSH D001926 | DiseasesDB 1572 | |
 | ||
Brain death is the complete and irreversible loss of brain function (including involuntary activity necessary to sustain life). Brain death is one of the two ways of determination of death, according to the Uniform Determination of Death Act of the United States (the other way of determining death being "irreversible cessation of circulatory and respiratory functions"). It differs from persistent vegetative state, in which the person is alive and some autonomic functions remain.
Contents
Brain death is used as an indicator of legal death in many jurisdictions, but it is defined inconsistently. Various parts of the brain may keep living when others die, and the term "brain death" has been used to refer to various combinations. For example, although a major medical dictionary says that "brain death" is synonymous with "cerebral death" (death of the cerebrum), the US National Library of Medicine Medical Subject Headings (MeSH) system defines brain death as including the brainstem. The distinctions can be important because, for example, in someone with a dead cerebrum but a living brainstem, the heartbeat and ventilation can continue unaided, whereas in whole-brain death (which includes brain stem death), only life support equipment would keep those functions going. Patients classified as brain-dead can have their organs surgically removed for organ donation.
Legal history
Traditionally, both the legal and medical communities determined death through the permanent end of certain bodily functions in clinical death, especially respiration and heartbeat. With the increasing ability of the medical community to resuscitate people with no respiration, heartbeat, or other external signs of life, the need for another definition of death occurred, raising questions of legal death. This gained greater urgency with the widespread use of life support equipment, as well as rising capabilities and demand for organ transplantation.
Since the 1960s, laws on determining death have, therefore, been implemented in all countries with active organ transplantation programs. The first European country to adopt brain death as a legal definition (or indicator) of death was Finland, in 1971. In the United States, Kansas had enacted a similar law earlier. In the 1970s, the Supreme Court of the state of New Jersey ruled that patients and their families have the right to decide when and whether to remove life support.
An ad hoc committee at Harvard Medical School published a pivotal 1968 report to define irreversible coma. The Harvard criteria gradually gained consensus toward what is now known as brain death. In the wake of the 1976 Karen Ann Quinlan case, state legislatures in the United States moved to accept brain death as an acceptable indication of death. In 1981 a Presidential commission issued a landmark report – Defining Death: Medical, Legal, and Ethical Issues in the Determination of Death – that rejected the "higher brain" approach to death in favor of a "whole brain" definition. This report was the basis for the Uniform Determination of Death Act, which has been enacted in 39 states of the United States the Uniform Determination of Death Act in the United States attempts to standardize criteria. Today, both the legal and medical communities in the US use "brain death" as a legal definition of death, allowing a person to be declared legally dead even if life support equipment keeps the body's metabolic processes working.
In the UK, the Royal College of Physicians reported in 1995, abandoning the 1979 claim that the tests published in 1976 sufficed for the diagnosis of brain death and suggesting a new definition of death based on the irreversible loss of brain stem function alone. This new definition, the irreversible loss of the capacity for consciousness and for spontaneous breathing, and the essentially unchanged 1976 tests held to establish that state, have been adopted as a basis of death certification for organ transplant purposes in subsequent Codes of Practice. The Australia and New Zealand Intensive Care Society (ANZICS) states that the "determination of brain death requires that there is unresponsive coma, the absence of brain-stem reflexes and the absence of respiratory centre function, in the clinical setting in which these findings are irreversible. In particular, there must be definite clinical or neuro-imaging evidence of acute brain pathology (e.g. traumatic brain injury, intracranial haemorrhage, hypoxic encephalopathy) consistent with the irreversible loss of neurological function."
Medical criteria
It is very important for family members and health care professionals to be aware of natural movements also known as Lazarus sign or Lazarus reflex that can occur on a brain-dead person whose organs have been kept functioning by life support. The living cells that can cause these movements are not living cells from the brain or brain stem, these cells come from the spinal cord. Sometimes these body movements can cause false hope for the family members.
A brain-dead individual has no clinical evidence of brain function upon physical examination. This includes no response to pain and no cranial nerve reflexes. Reflexes include pupillary response (fixed pupils), oculocephalic reflex, corneal reflex, no response to the caloric reflex test, and no spontaneous respirations.
It is important to distinguish between brain death and states that may be difficult to differentiate from brain death, (such as barbiturate overdose, alcohol intoxication, sedative overdose, hypothermia, hypoglycemia, coma, and chronic vegetative states). Some comatose patients can recover to pre-coma or near pre-coma level of functioning, and some patients with severe irreversible neurological dysfunction will nonetheless retain some lower brain functions, such as spontaneous respiration, despite the losses of both cortex and brain stem functionality. Such is the case with anencephaly.
Note that brain electrical activity can stop completely, or drop to such a low level as to be undetectable with most equipment. An EEG will therefore be flat, though this is sometimes also observed during deep anesthesia or cardiac arrest. Although in the United States a flat EEG test is not required to certify death, it is considered to have confirmatory value. In the UK it is not considered to be of value because any continuing activity it might reveal in parts of the brain above the brain stem is held to be irrelevant to the diagnosis of death on the Code of Practice criteria.
The diagnosis of brain death needs to be rigorous, in order to be certain that the condition is irreversible. Legal criteria vary, but in general they require neurological examinations by two independent physicians. The exams must show complete and irreversible absence of brain function (brain stem function in UK), and may include two isoelectric (flat-line) EEGs 24 hours apart (less in other countries where it is accepted that if the cause of the dysfunction is a clear physical trauma there is no need to wait that long to establish irreversibility). The patient should have a normal temperature and be free of drugs that can suppress brain activity if the diagnosis is to be made on EEG criteria.
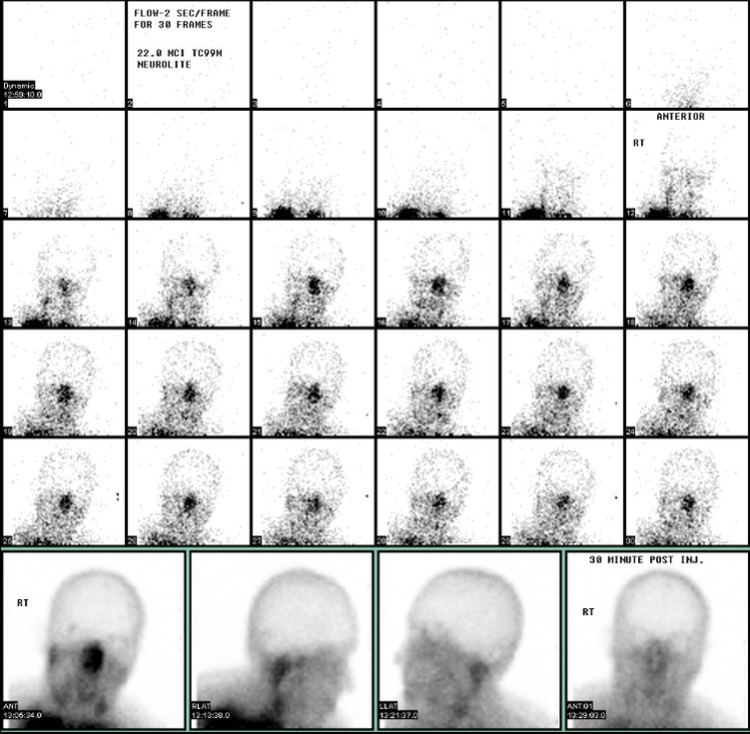
Also, a radionuclide cerebral blood flow scan that shows complete absence of intracranial blood flow must be considered with other exams – temporary swelling of the brain, particularly within the first 72 hours, can lead to a false positive test on a patient that may recover with more time.
CT angiography is neither required nor sufficient test to make the diagnosis.
Organ donation
While the diagnosis of brain death has become accepted as a basis for the certification of death for legal purposes, it should be clearly understood that it is a very different state from biological death - the state universally recognized and understood as death. The continuing function of vital organs in the bodies of those diagnosed brain dead, if mechanical ventilation and other life-support measures are continued, provides optimal opportunities for their transplantation.
When mechanical ventilation is used to support the body of a brain dead organ donor pending a transplant into an organ recipient, the donor's date of death is listed as the date that brain death was diagnosed.
In some countries (for instance, Spain, Finland, Poland, Wales, Portugal, and France), everyone is automatically an organ donor after diagnosis of death on legally accepted criteria, although some jurisdictions (such as Singapore, Spain, Wales, France, Czech Republic and Portugal) allow opting out of the system. Elsewhere, consent from family members or next-of-kin may be required for organ donation. In New Zealand, Australia, the United Kingdom (excluding Wales) and most states in the United States, drivers are asked upon application if they wish to be registered as an organ donor.
In the United States, if the patient is at or near death, the hospital must notify a transplant organization of the person's details and maintain the patient while the patient is being evaluated for suitability as a donor. The patient is kept on ventilator support until the organs have been surgically removed. If the patient has indicated in an advance health care directive that they do not wish to receive mechanical ventilation or has specified a do not resuscitate order and the patient has also indicated that they wish to donate their organs, some vital organs such as the heart and lungs may not be able to be recovered.
