ICD-10 E51.1 DiseasesDB 14107 eMedicine ped/229 med/221 | ICD-9-CM 265.0 MedlinePlus 000339 | |
 | ||
Specialty Neurology, cardiology, pediatrics | ||
Beriberi refers to a cluster of symptoms caused primarily by thiamine (vitamin B1) deficiency. Beriberi has conventionally been divided into three separate entities, relating to the body system mainly involved (peripheral nervous system or cardiovascular) or age of person (like infantile). Beriberi is one of several thiamine-deficiency related conditions, which may occur concurrently, including Wernicke's encephalopathy (mainly affecting the central nervous system), Korsakoff's syndrome (amnesia with additional psychiatric manifestations), and Wernicke-Korsakoff syndrome (with both neurologic and psychiatric symptoms).
Contents
- Signs and symptoms
- Dry beriberi
- Wet beriberi
- Infantile beriberi
- Gastrointestinal beriberi
- Cause
- Pathophysiology
- Treatment
- Epidemiology
- Etymology
- Identification
- References
Historically, beriberi has been common in regions where what is variously referred to as polished or white rice forms a major part of the diet, which has its husk removed to extend its shelf life and palatability but has the side effect of removing the primary source of thiamine. It was not known until the end of the 19th century that polishing rice was associated with beriberi.
Signs and symptoms
Symptoms of beriberi include weight loss, emotional disturbances, impaired sensory perception, weakness and pain in the limbs, and periods of irregular heart rate. Edema (swelling of bodily tissues) is common. It may increase the amount of lactic acid and pyruvic acid within the blood. In advanced cases, the disease may cause high-output cardiac failure and death. Symptoms may occur concurrently with those of Wernicke's encephalopathy, a primarily neurological thiamine-deficiency related condition.
Beriberi is divided into four categories as follows. The first three are historical and the fourth, gastrointestinal beriberi, was recognized in 2004:
Dry beriberi
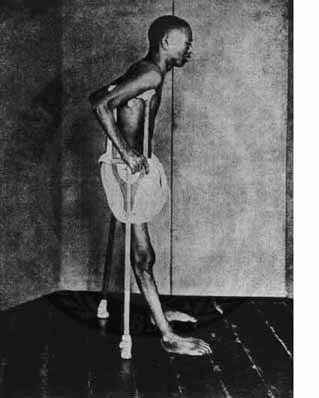
Dry beriberi causes wasting and partial paralysis resulting from damaged peripheral nerves. It is also referred to as endemic neuritis. It is characterized by:
A selective impairment of the large proprioceptive sensory fibers without motor impairment can occur and present as a prominent sensory ataxia, which is a loss of balance and coordination due to loss of the proprioceptive inputs from the periphery and loss of position sense.
Wet beriberi
Wet beriberi affects the heart and circulatory system. It is sometimes fatal, as it causes a combination of heart failure and weakening of the capillary walls, which causes the peripheral tissues to become edematous. Wet beriberi is characterized by:
Infantile beriberi
Infantile beriberi usually occurs between two and six months of age in children whose mothers have inadequate thiamine intake. In the acute form, the baby develops dyspnea and cyanosis and soon dies of heart failure. These symptoms may be described in infantile beriberi:
Gastrointestinal beriberi
Gastrointestinal beriberi causes abdominal pain. Gastrointestinal beriberi is characterized by:
Cause
Beriberi may also be caused by shortcomings other than inadequate intake: diseases or operations on the digestive tract, alcoholism, dialysis, genetic deficiencies, etc. All these causes mainly affecting the central nervous system, and provoking the development of what is known as Wernicke's disease or Wernicke's encephalopathy.
Wernicke´s disease is one of the most prevalent neurological or neuropsychiatric diseases. In autopsy series, features of Wernicke lesions are observed in approximately 2% of general cases. Medical record research shows that about 85% had not been diagnosed, although only 19% would be asymptomatic. In children, only 58% were diagnosed. In alcohol abusers, autopsy series showed neurological damages at rates of 12.5% or more. Mortality caused by Wernicke's disease reaches 17% of diseases, which means 3.4/1000 or about 25 million contemporaries. The number of people with Wernicke's disease may be even higher, considering that early stages may have dysfunctions prior to the production of observable lesions at necropsy. In addition, uncounted numbers of people can experience fetal damage and subsequent diseases.
Pathophysiology
Thiamine in the human body has a half-life of 18 days and is quickly exhausted, particularly when metabolic demands exceed intake. A derivative of thiamine, thiamine pyrophosphate (TPP), is a cofactor involved in the citric acid cycle, as well as connecting the breakdown of sugars with the citric acid cycle. The citric acid cycle is a central metabolic pathway involved in the regulation of carbohydrate, lipid, and amino acid metabolism, and its disruption due to thiamine deficiency inhibits the production of many molecules including the neurotransmitters glutamic acid and GABA. Additionally thiamine may also be directly involved in neuromodulation.
Treatment
Many people with beriberi can be treated with thiamine alone. Given thiamine intravenously (and later orally), rapid and dramatic recovery can occur within hours. In situations where concentrated thiamine supplements are unavailable, feeding the person with a thiamine-rich diet (e.g. whole grain brown bread) will lead to recovery, though at a much slower rate.
Epidemiology
Historically beriberi was associated with a diet including much polished rice; when the relationship between polishing rice and the disease was discovered, it became possible to prevent and treat the deficiency condition, for example with inexpensive rice bran. Beriberi caused by inadequate nutritional intake is rare today in developed countries because of quality of food and the fact that many foods are fortified with vitamins. No reliable statistics are given for beriberi in developed countries in the 19th century or earlier; neither are statistics available before the last century in countries in extreme poverty.
Beriberi is a recurrent nutritional disease in detention houses even in this century. In 1999, an outbreak of beriberi occurred in a detention center in Taiwan. High rates of illness and death in overcrowded Haitian jails were traced in 2007 to the traditional practice of washing rice before cooking. In the Ivory Coast, among a group of prisoners with heavy punishment, 64% were affected by beriberi. Before beginning treatment, prisoners exhibited symptoms of dry or wet beriberi with neurological signs (swarming: 41%), cardiovascular signs (dyspnoea: 42%, thoracic pain: 35%), and oedemas of the lower limbs (51%). With treatment the rate of healing was about 97%.
Populations under extreme stress may be at higher risk for beriberi. Displaced populations, such as refugees from war, are susceptible to micronutritional deficiency, including beriberi. The severe nutritional deprivation caused by famine also can cause beriberis, although symptoms may be overlooked in clinical assessment or masked by other famine-related problems. An extreme weight-loss diet can, rarely, induce a famine-like state and the accompanying beriberi.
Etymology
According to the Oxford English Dictionary, the term 'beriberi' comes from a Sinhalese phrase meaning "weak, weak" or "I cannot, I cannot", the word being duplicated for emphasis.
According to Jacobus Bontius (Jacob de Bondt; 1591–1631), a Dutch physician who encountered the disease while working in Java in 1630, the word came from Malay word, biri-biri. In the first known description of beriberi (or, beri-beri), he wrote: "A certain very troublesome affliction, which attacks men, is called by the inhabitants beriberi (which means sheep). I believe those, whom this same disease attacks, with their knees shaking and the legs raised up, walk like sheep. It is a kind of paralysis, or rather tremor: for it penetrates the motion and sensation of the hands and feet indeed sometimes of the whole body."
Identification
In the late 19th century, beriberi was studied by Takaki Kanehiro, a British-trained Japanese medical doctor of the Japanese Navy. Beriberi was a serious problem in the Japanese navy: sailors fell ill an average of four times a year in the period 1878 to 1881, and 35% were cases of beriberi. In 1883, Kanehiro learned of a very high incidence of beriberi among cadets on a training mission from Japan to Hawaii, via New Zealand and South America. The voyage lasted more than 9 months and resulted in 169 cases of sickness and 25 deaths on a ship of 376 men. With the support of the Japanese Navy, he conducted an experiment in which another ship was deployed on the same route, except that its crew was fed a diet of meat, fish, barley, rice, and beans. At the end of the voyage, this crew had only 14 cases of beriberi and no deaths. This convinced Kanehiro and the Japanese Navy that diet was the cause. In 1884, Kanehiro observed that beriberi was endemic among low-ranking crew who were often provided free rice and thus ate little else, but not among crews of Western navies and nor among Japanese officers who consumed a more varied diet.
In 1897, Christiaan Eijkman, a Dutch physician and pathologist, demonstrated that beriberi is caused by poor diet, and discovered that feeding unpolished rice (instead of the polished variety) to chickens helped to prevent beriberi. The following year, Sir Frederick Hopkins postulated that some foods contained "accessory factors" – in addition to proteins, carbohydrates, fats, and salt – that were necessary for the functions of the human body. In 1901, Gerrit Grijns (May 28, 1865 – November 11, 1944), a Dutch physician and assistant to Christiaan Eijkman in the Netherlands, correctly interpreted the disease as a deficiency syndrome, and between 1910 and 1913, Edward Bright Vedder established that an extract of rice bran is a treatment for beriberi. In 1929, Eijkman and Hopkins were awarded the Nobel Prize for Physiology or Medicine for their discoveries.
