ICD-9-CM 427.32 MedlinePlus 000184 | ICD-10 I48 DiseasesDB 1072 eMedicine med/185 | |
 | ||
Atrial flutter (AFL) is a common abnormal heart rhythm that starts in the atrial chambers of the heart. When it first occurs, it is usually associated with a fast heart rate (100 or more heartbeats per minute), and is classified as a type of supra-ventricular tachycardia. Although this abnormal heart rhythm typically occurs in individuals with cardiovascular disease (e.g. high blood pressure, coronary artery disease, and cardiomyopathy) and diabetes mellitus, it may occur spontaneously in people with otherwise normal hearts. It is typically not a stable rhythm, and often degenerates into atrial fibrillation (AF). However, it does rarely persist for months to years.
Contents
- Signs and symptoms
- Pathophysiology
- Classification
- Type I
- Type II
- Management
- Cardioversion
- Ablation
- Complications
- Rate related
- Clot formation
- Sudden cardiac death
- References
Atrial flutter was first identified as an independent medical condition in 1920 by the British physician Sir Thomas Lewis (1881–1945) and colleagues.
Signs and symptoms
While atrial flutter can sometimes go unnoticed, its onset is often marked by characteristic sensations of regular palpitations. Such sensations usually last until the episode resolves, or until the heart rate is controlled.
Atrial flutter is usually well tolerated initially (a high heart rate is for most people just a normal response to exercise), however, people with other underlying heart disease or poor exercise tolerance may rapidly develop symptoms, which can be shortness of breath, chest pains, lightheadedness or dizziness, nausea and, in some patients, nervousness and feelings of impending doom.
Prolonged fast flutter may lead to decompensation with loss of normal heart function (heart failure). This may manifest as effort intolerance (exertional breathlessness), nocturnal breathlessness, or swelling of the legs or abdomen.
Atrial flutter is recognized on an electrocardiogram by presence of characteristic flutter waves at a regular rate of 280 to 300 beats per minute. Individual flutter waves may be symmetrical, resembling p-waves, or may be asymmetrical with a "sawtooth" shape, rising gradually and falling abruptly or vice versa. If atrial flutter is suspected clinically but is not clearly evident on ECG, acquiring a Lewis lead ECG may be helpful in revealing flutter waves.
Pathophysiology
Atrial flutter is caused by a re-entrant rhythm in either the right or left atrium. Typically initiated by a premature electrical impulse arising in the atria, atrial flutter is propagated due to differences in refractory periods of atrial tissue. This creates electrical activity that moves in a localized self-perpetuating loop. For each cycle around the loop, there results an electric impulse that propagates through the atria.
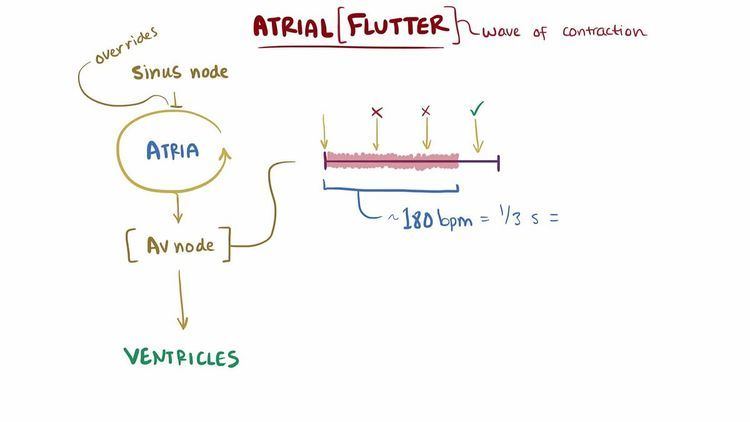
The impact and symptoms of atrial flutter depend on the heart rate of the patient. Heart rate is a measure of the ventricular rather than atrial activity. Impulses from the atria are conducted to the ventricles through the atrio-ventricular node (AV node). Due primarily to its longer refractory period, the AV node exerts a protective effect on heart rate by blocking atrial impulses in excess of about 180 beats/minute, for the example of a resting heart rate. (This block is dependent on the age of the patient, and can be calculated roughly by subtracting patient age from 220). If the flutter rate is 300/minute only half of these impulses will be conducted, giving a ventricular rate of 150/minute, or a 2:1 heart block. The addition of rate-controlling drugs or conduction system disease can increase this block substantially (see image below).
Classification
There are two types of atrial flutter, the common type I and rarer type II. Most individuals with atrial flutter will manifest only one of these. Rarely someone may manifest both types; however, they can only manifest one type at a time.
Type I
Type I atrial flutter, also known as common atrial flutter or typical atrial flutter, has an atrial rate of 240 to 340 beats/minute. However, this rate may be slowed by antiarrhythmic agents.
The reentrant loop circles the right atrium, passing through the cavo-tricuspid isthmus - a body of fibrous tissue in the lower atrium between the inferior vena cava, and the tricuspid valve. Type I flutter is further divided into two subtypes, known as counterclockwise atrial flutter and clockwise atrial flutter depending on the direction of current passing through the loop.
Catheter ablation of the isthmus is a procedure usually available in the electrophysiology laboratory. Eliminating conduction through the isthmus prevents reentry, and if successful, prevents the recurrence of the atrial flutter.
Type II
Type II flutter follows a significantly different re-entry pathway to type I flutter, and is typically faster, usually 340-440 beats/minute. Left atrial flutter is common after incomplete left atrial ablation procedures.
Management
In general, atrial flutter should be managed the same as atrial fibrillation. Because both rhythms can lead to the formation of a blood clot in the atrium, individuals with atrial flutter usually require some form of anticoagulation or antiplatelet agent. Both rhythms can be associated with dangerously fast heart rates and thus require medication to control the heart rate (such as beta blockers or calcium channel blockers) and/or rhythm control (such as ibutilide or dofetilide). However, atrial flutter is more resistant to correction with such medications than atrial fibrillation. For example, although the class III antiarrhythmic agent ibutilide is an effective treatment for atrial flutter, rates of recurrence after treatment are quite high (70-90%). Additionally, there are some specific considerations particular to treatment of atrial flutter.
Cardioversion
Atrial flutter is considerably more sensitive to electrical direct-current cardioversion than atrial fibrillation, with a shock of only (20 to 50) J commonly being enough to cause a return to sinus rhythm. Exact placement of the pads does not appear important.
Ablation
Due to the reentrant nature of atrial flutter, it is often possible to ablate the circuit that causes atrial flutter with radiofrequency catheter ablation. This is done in the electrophysiology lab by causing a ridge of scar tissue that crosses the path of the circuit that causes atrial flutter. Ablation of the isthmus, as discussed above, is a common treatment for typical atrial flutter.
Complications
Although often regarded as a relatively benign rhythm problem, atrial flutter shares the same complications as the related condition atrial fibrillation. There is paucity of published data directly comparing the two, but overall mortality in these conditions appears to be very similar.
Rate related
Rapid heart rates may produce significant symptoms in patients with pre-existing heart disease and can lead to inadequate blood flow to the heart muscle and even a heart attack. In rare situations, atrial flutter associated with a fast heart rate persists for an extended period of time without being corrected to a normal heart rhythm and leads to a tachycardia-induced cardiomyopathy. Even in patients whose hearts are normal to start with, prolonged tachycardia tends to produce ventricular decompensation and heart failure.
Clot formation
Because there is little if any effective contraction of the atria there is stasis (pooling) of blood in the atria. Stasis of blood in susceptible individuals can lead to the formation of a thrombus (blood clot) within the heart. Thrombus is most likely to form in the atrial appendages. A blood clot in the left atrial appendage is particularly important as the left side of the heart supplies blood to the entire body. Thus, any thrombus material that dislodges from this side of the heart can embolize to the brain, with the potentially devastating consequence of a stroke. Thrombus material can, of course, embolize to any other portion of the body, though usually with a less severe outcome.
Sudden cardiac death
Sudden death is not directly associated with atrial flutter. However, in individuals with a pre-existing accessory conduction pathway, such as the bundle of Kent in Wolff-Parkinson-White syndrome, the accessory pathway may conduct activity from the atria to the ventricles at a rate that the AV node would usually block. Bypassing the AV node, the atrial rate of 300 beats/minute leads to a ventricular rate of 300 beats/minute (1:1 conduction). Even if the ventricles are able to sustain a cardiac output at such a high rates, 1:1 flutter with time may degenerate into ventricular fibrillation, causing hemodynamic collapse and death.
