Specialty toxicology | ||
 | ||
Symptoms Treatment dimercaptosuccinic acid, dimercaptopropane sulfonate | ||
Arsenic poisoning is a medical condition that occurs due to elevated levels of arsenic in the body. If exposure occurs over a brief period of time symptoms may include vomiting, abdominal pain, encephalopathy, and watery diarrhea that contains blood. Long-term exposure can result in thickening of the skin, darker skin, abdominal pain, diarrhea, heart disease, numbness, and cancer.
Contents
- Signs and symptoms
- Cancer
- Causes
- Drinking water
- Occupational exposures
- Food
- Pathophysiology
- Mechanism
- Kinetics
- Heat shock response
- Oxidative stress
- Diagnosis
- Chelation
- Nutrition
- History
- Notable cases
- Francesco I de Medici Grand Duke of Tuscany
- Eric XIV of Sweden
- George III of Great Britain
- Theodor Ursinus
- Napoleon Bonaparte
- Simn Bolvar
- Charles Francis Hall
- Clare Boothe Luce
- Guangxu Emperor
- Phar Lap
- King Faisal I of Iraq
- Anderson Mazoka
- References
The most common reason for long-term exposure is contaminated drinking water. Groundwater most often becomes contaminated naturally; however, contamination may also occur from mining or agriculture. Recommended levels in water are less than 10–50 ug/l (10–50 parts per billion). Other routes of exposure include toxic waste sites and traditional medicines. Most cases of poisoning are accidental. Arsenic acts via changing the functioning of around 200 enzymes. Diagnosis is by testing the urine, blood, or hair.
Prevention is by using water that does not contain high levels of arsenic. This may be achieved by the use of special filters or using rainwater. There is not good evidence to support specific treatments for long-term poisoning. For acute poisonings treating dehydration is important. Dimercaptosuccinic acid (DMSA) or dimercaptopropane sulfonate (DMPS) may be used while dimercaprol (BAL) is not recommended. Hemodialysis may also be used.
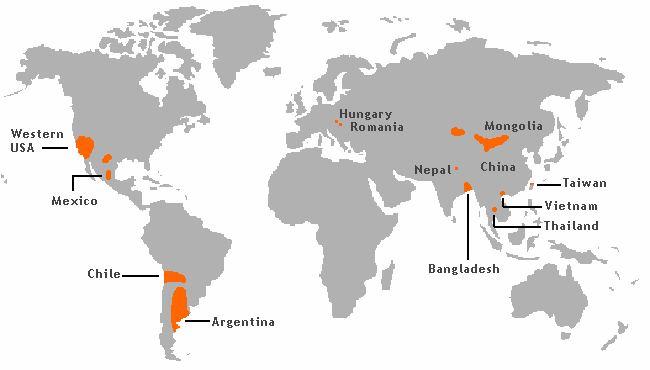
Through drinking water, more than 200 million people globally are exposed to higher than safe levels of arsenic. The areas most affected are Bangladesh and West Bengal. Acute poisoning is uncommon. The toxicity of arsenic has been described as far back as 1500 BC in the Ebers papyrus.
Signs and symptoms
Symptoms of arsenic poisoning begin with headaches, confusion, severe diarrhea, and drowsiness. As the poisoning develops, convulsions and changes in fingernail pigmentation called leukonychia striata (Mees's lines, or Aldrich-Mees's lines) may occur. When the poisoning becomes acute, symptoms may include diarrhea, vomiting, vomiting blood, blood in the urine, cramping muscles, hair loss, stomach pain, and more convulsions. The organs of the body that are usually affected by arsenic poisoning are the lungs, skin, kidneys, and liver. The final result of arsenic poisoning is coma and death.
Arsenic is related to heart disease (hypertension-related cardiovascular disease), cancer, stroke (cerebrovascular diseases), chronic lower respiratory diseases, and diabetes.
Chronic exposure to arsenic is related to vitamin A deficiency, which is related to heart disease and night blindness.
Inorganic arsenites (arsenic(III)) in drinking water have a much higher acute toxicity than organic arsenates (arsenic(V)). The acute minimal lethal dose of arsenic in adults is estimated to be 70 to 200 mg or 1 mg/kg/day.
Cancer
Arsenic increases the risk of cancer. Exposure is related to skin, lung, liver, and kidney cancer among others.
Its comutagenic effects may be explained by interference with base and nucleotide excision repair, eventually through interaction with zinc finger structures. Dimethylarsinic acid, DMA(V), caused DNA single stand breaks resulting from inhibition of repair enzymes at levels of 5 to 100 mM in human epithelial type II cells.
MMA(III) and DMA(III) were also shown to be directly genotoxic by effectuating scissions in supercoiled ΦX174 DNA. Increased arsenic exposure is associated with an increased frequency of chromosomal aberrations, micronuclei and sister-chromatid exchanges. An explanation for chromosomal aberrations is the sensitivity of the protein tubulin and the mitotic spindle to arsenic. Histological observations confirm effects on cellular integrity, shape and locomotion.
DMA(III) is able to form reactive oxygen species (ROS) by reaction with molecular oxygen. Resulting metabolites are the dimethylarsenic radical and the dimethylarsenic peroxyl radical. Both DMA(III) and DMA(V) were shown to release iron from horse spleen as well as from human liver ferritin if ascorbic acid was administered simultaneously. Thus, formation of ROS can be promoted. Moreover, arsenic could cause oxidative stress by depleting the cell’s antioxidants, especially the ones containing thiol groups. The accumulation of ROS like the cited above and hydroxyl radicals, superoxide radicals and hydrogen peroxides causes aberrant gene expression at low concentrations and lesions of lipids, proteins and DNA in higher concentrations which eventually lead to cellular death. In a rat animal model, urine levels of 8-hydroxy-2’-desoxyguanosine (as a biomarker of ROS DNA damage) were measured after treatment with DMA(V). In comparison to control levels, they turned out to be significantly increased. This theory is further supported by a cross-sectional study which found elevated mean serum lipid peroxides (LPO) in the As exposed individuals which correlated with blood levels of inorganic arsenic and methylated metabolites and inversely correlated with nonprotein sulfhydryl (NPSH) levels in whole blood. Another study found an association of As levels in whole blood with the level of reactive oxidants in plasma and an inverse relationship with plasma antioxidants. A finding of the latter study indicates that methylation might in fact be a detoxification pathway with regard to oxidative stress: the results showed that the lower the As methylation capacity was, the lower the level of plasma antioxidant capacity. As reviewed by Kitchin (2001), the oxidative stress theory provides an explanation for the preferred tumor sites connected with arsenic exposure. Considering that a high partial pressure of oxygen is present in lungs and DMA(III) is excreted in gaseous state via the lungs this seems to be a plausible mechanism for special vulnerability. The fact that DMA is produced by methylation in the liver, excreted via the kidneys and latter on stored in the bladder accounts for the other tumor localizations.
Regarding DNA methylation, some studies suggest interaction of As with methyltransferases which leads to an inactivation of tumor suppressor genes through hypermethylation, others state that hypomethylation might occur due to a lack of SAM resulting in aberrant gene activation. An experiment by Zhong et al. (2001) with arsenite-exposed human lung A549, kidney UOK123, UOK109 and UOK121 cells isolated eight different DNA fragments by methylation-sensitive arbitrarily primed PCR. It turned out that six of the fragments were hyper- and two of them were hypomethylated. Higher levels of DNA methltransferase mRNA and enzyme activity were found.
Kitchin (2001) proposed a model of altered growth factors which lead to cell proliferation and thus to carcinogenesis. From observations, it is known that chronic low-dose arsenic poisoning can lead to increased tolerance to its acute toxicity. MRP1-overexpressing lung tumor GLC4/Sb30 cells poorly accumulate arsenite and arsenate. This is mediated through MRP-1 dependent efflux. The efflux requires GSH, but no As-GSH complex formation.
Although many mechanisms have been proposed, no definite model can be given for the mechanisms of chronic arsenic poisoning. The prevailing events of toxicity and carcinogenicity might be quite tissue-specific. Current consensus on the mode of carcinogenesis is that it acts primarily as a tumor promoter. Its co-carcinogenicity has been demonstrated in several models. However, the finding of several studies that chronically arsenic-exposed Andean populations (as most extremely exposed to UV-light) do not develop skin cancer with chronic arsenic exposure, is puzzling.
Causes
Organic arsenic is less harmful than inorganic arsenic. Seafood is a common source of the less toxic organic arsenic in the form of arsenobetaine. The arsenic reported in 2012 in fruit juice and rice by Consumer Reports was primarily inorganic arsenic.
Drinking water
Chronic arsenic poisoning results from drinking contaminated well water over a long period of time. Many aquifers contain high concentration of arsenic salts. The World Health Organization (WHO) recommends a limit of 0.01 mg/L (10 parts per billion) of arsenic in drinking water. This recommendation was established based on the limit of detection for most laboratories' testing equipment at the time of publication of the WHO water quality guidelines. More recent findings show that consumption of water with levels as low as 0.00017 mg/L (0.17 parts per billion) over long periods of time can lead to arsenicosis.
From a 1988 study in China, the US protection agency quantified the lifetime exposure of arsenic in drinking water at concentrations of 0.0017 mg/L, 0.00017 mg/L, and 0.000017 mg/L are associated with a lifetime skin cancer risk of 1 in 10,000, 1 in 100,000, and 1 in 1,000,000 respectively. WHO asserts that a level of 0.01 mg/L poses a risk of 6 in 10000 chance of lifetime skin cancer risk and contends that this level of risk is acceptable.
One of the worst incidents of arsenic poisoning via well water occurred in Bangladesh, which the World Health Organization called the "largest mass poisoning of a population in history."
Mining techniques such as hydraulic fracturing may mobilize arsenic in groundwater and aquifers due to enhanced methane transport and resulting changes in redox conditions, and inject fluid containing additional arsenic.
Occupational exposures
Because of its high toxicity, arsenic is seldom used in the Western world, although in Asia it is still a popular pesticide. Arsenic is mainly encountered occupationally in the smelting of zinc and copper ores.
Food
It has been found that rice is particularly susceptible to accumulation of arsenic from soil. Rice grown in the U.S. has an average 260 ppb of arsenic, according to a study; but U.S. arsenic intake remains far below World Health Organization-recommended limits. China has set a standard for arsenic limits in food (150 ppb), as levels in rice exceed those in water.
Arsenic is a ubiquitous element present in American drinking water. In the United States, levels of arsenic that are above natural levels, but still well below danger levels set in federal safety standards, have been detected in commercially grown chickens. The source of the arsenic appears to be the feed additives roxarsone and nitarsone, which are used to control the parasitic infection coccidiosis as well as to increase weight and skin coloring of the poultry.
High levels of inorganic arsenic were reportedly found in 83 California wines in 2015.
Pathophysiology
Arsenic interferes with cellular longevity by allosteric inhibition of an essential metabolic enzyme pyruvate dehydrogenase (PDH) complex, which catalyzes the oxidation of pyruvate to acetyl-CoA by NAD+. With the enzyme inhibited, the energy system of the cell is disrupted resulting in a cellular apoptosis episode. Biochemically, arsenic prevents use of thiamine resulting in a clinical picture resembling thiamine deficiency. Poisoning with arsenic can raise lactate levels and lead to lactic acidosis. Low potassium levels in the cells increases the risk of experiencing a life-threatening heart rhythm problem from arsenic trioxide. Arsenic in cells clearly stimulates the production of hydrogen peroxide (H2O2). When the H2O2 reacts with certain metals such as iron or manganese it produces a highly reactive hydroxyl radical. Inorganic arsenic trioxide found in ground water particularly affects voltage-gated potassium channels, disrupting cellular electrolytic function resulting in neurological disturbances, cardiovascular episodes such as prolonged QT interval, neutropenia, high blood pressure, central nervous system dysfunction, anemia, and death.
Arsenic exposure plays a key role in the pathogenesis of vascular endothelial dysfunction as it inactivates endothelial nitric oxide synthase, leading to reduction in the generation and bioavailability of nitric oxide. In addition, the chronic arsenic exposure induces high oxidative stress, which may affect the structure and function of cardiovascular system. Further, the arsenic exposure has been noted to induce atherosclerosis by increasing the platelet aggregation and reducing fibrinolysis. Moreover, arsenic exposure may cause arrhythmia by increasing the QT interval and accelerating the cellular calcium overload. The chronic exposure to arsenic upregulates the expression of tumor necrosis factor-α, interleukin-1, vascular cell adhesion molecule and vascular endothelial growth factor to induce cardiovascular pathogenesis.
Tissue culture studies have shown that arsenic compounds block both IKr and Iks channels and, at the same time, activates IK-ATP channels. Arsenic compounds also disrupt ATP production through several mechanisms. At the level of the citric acid cycle, arsenic inhibits pyruvate dehydrogenase and by competing with phosphate it uncouples oxidative phosphorylation, thus inhibiting energy-linked reduction of NAD+, mitochondrial respiration, and ATP synthesis. Hydrogen peroxide production is also increased, which might form reactive oxygen species and oxidative stress. These metabolic interferences lead to death from multi-system organ failure, probably from necrotic cell death, not apoptosis. A post mortem reveals brick red colored mucosa, due to severe hemorrhage. Although arsenic causes toxicity, it can also play a protective role.
Mechanism
Arsenite inhibits not only the formation of acetyl-CoA but also the enzyme succinic dehydrogenase. Arsenate can replace phosphate in many reactions. It is able to form Glc-6-Arsenate in vitro; therefore it has been argued that hexokinase could be inhibited. (Eventually this may be a mechanism leading to muscle weakness in chronic arsenic poisoning.) In the glyceraldehyde 3-phosphate dehydrogenase reaction arsenate attacks the enzyme-bound thioester. The formed 1-arseno-3-phosphoglycerate is unstable and hydrolyzes spontaneously. Thus, ATP formation in Glycolysis is inhibited while bypassing the phosphoglycerate kinase reaction. (Moreover, the formation of 2,3-bisphosphoglycerate in erythrocytes might be affected, followed by a higher oxygen affinity of hemoglobin and subsequently enhanced cyanosis) As shown by Gresser (1981), submitochondrial particles synthesize Adenosine-5’-diphosphate-arsenate from ADP and arsenate in presence of succinate. Thus, by a variety of mechanisms arsenate leads to an impairment of cell respiration and subsequently diminished ATP formation. This is consistent with observed ATP depletion of exposed cells and histopathological findings of mitochondrial and cell swelling, glycogen depletion in liver cells and fatty change in liver, heart and kidney.
Experiments demonstrated enhanced arterial thrombosis in a rat animal model, elevations of serotonin levels, thromboxane A[2] and adhesion proteins in platelets, while human platelets showed similar responses. The effect on vascular endothelium may eventually be mediated by the arsenic-induced formation of nitric oxide. It was demonstrated that +3 As concentrations substantially lower than concentrations required for inhibition of the lysosomal protease cathepsin L in B cell line TA3 were sufficient to trigger apoptosis in the same B cell line, while the latter could be a mechanism mediating immunosuppressive effects.
Kinetics
The two forms of inorganic arsenic, reduced (trivalent As (III)) and oxidized (pentavalent As(V)), can be absorbed, and accumulated in tissues and body fluids. In the liver, the metabolism of arsenic involves enzymatic and non-enzymatic methylation, the most frequently excreted metabolite (≥ 90%) in the urine of mammals is dimethylarsinic acid or cacodylic acid, DMA(V). Dimethylarsenic acid is also known as Agent Blue and was used as herbicide in the American war in Vietnam.
In humans inorganic arsenic is reduced nonenzymatically from pentoxide to trioxide, using glutathione (GSH) or it is mediated by enzymes. Reduction of arsenic pentoxide to arsenic trioxide increases its toxicity and bio availability, Methylation occurs through methyltransferase enzymes. S-adenosylmethionine (SAM) may serve as methyl donor. Various pathways are used, the principal route being dependent on the current environment of the cell. Resulting metabolites are monomethylarsonous acid, MMA(III), and dimethylarsinous acid, DMA(III).
Methylation had been regarded as a detoxification process, but reduction from +5 As to +3 As may be considered as a bioactivation instead. Another suggestion is that methylation might be a detoxification if "As[III] intermediates are not permitted to accumulate" because the pentavalent organoarsenics have a lower affinity to thiol groups than inorganic pentavalent arsenics. Gebel (2002) stated that methylation is a detoxification through accelerated excretion. With regard to carcinogenicity it has been suggested that methylation should be regarded as a toxification.
Arsenic, especially +3 As, binds to single, but with higher affinity to vicinal sulfhydryl groups, thus reacts with a variety of proteins and inhibits their activity. It was also proposed that binding of arsenite at nonessential sites might contribute to detoxification. Arsenite inhibits members of the disulfide oxidoreductase family like glutathione reductase and thioredoxin reductase.
The remaining unbound arsenic (≤ 10%) accumulates in cells, which over time may lead to skin, bladder, kidney, liver, lung, and prostate cancers. Other forms of arsenic toxicity in humans have been observed in blood, bone marrow, cardiac, central nervous system, gastrointestinal, gonadal, kidney, liver, pancreatic, and skin tissues.
Heat shock response
Another aspect is the similarity of arsenic effects to the heat shock response. Short-term arsenic exposure has effects on signal transduction inducing heat shock proteins with masses of 27,60,70,72,90,110 kDa as well as metallotionein, ubiquitin, mitogen-activated [MAP] kinases, extracellular regulated kinase [ERK], c-jun terminal kinases [JNK] and p38. Via JNK and p38 it activates c-fos, c-jun and egr-1 which are usually activated by growth factors and cytokines The effects are largely dependent on the dosing regime and may be as well inversed.
As shown by some experiments reviewed by Del Razo (2001), ROS induced by low levels of inorganic arsenic increase the transcription and the activity of the activator protein 1 (AP-1) and the nuclear factor-κB (NF-κB) (maybe enhanced by elevated MAPK levels), which results in c-fos/c-jun activation, over-secretion of pro-inflammatory and growth promoting cytokines stimulating cell proliferation. Germolec et al. (1996) found an increased cytokine expression and cell proliferation in skin biopsies from individuals chronically exposed to arsenic-contaminated drinking water.
Increased AP-1 and NF-κB obviously also result in an up-regulation of mdm2 protein, which decreases p53 protein levels. Thus, taking into account p53’s function, a lack of it could cause a faster accumulation of mutations contributing to carcinogenesis. However, high levels of inorganic arsenic inhibit NF-κB activation and cell proliferation. An experiment of Hu et al. (2002) demonstrated increased binding activity of AP-1 and NF-κB after acute (24 h) exposure to +3 sodium arsenite, whereas long-term exposure (10–12 weeks) yielded the opposite result. The authors conclude that the former may be interpreted as a defense response while the latter could lead to carcinogenesis. As the contradicting findings and connected mechanistic hypotheses indicate, there is a difference in acute and chronic effects of arsenic on signal transduction which is not clearly understood yet.
Oxidative stress
Studies have demonstrated that the oxidative stress generated by arsenic may disrupt the signal transduction pathways of the nuclear transcriptional factors PPAR’s, AP-1, and NF-κB, as well as the pro-inflammatory cytokines IL-8 and TNF-α. The interference of oxidative stress with signal transduction pathways may affect physiological processes associated with cell growth, metabolic syndrome X, glucose homeostasis, lipid metabolism, obesity, insulin resistance, inflammation, and diabetes-2. Recent scientific evidence has elucidated the physiological roles of the PPAR’s in the ω- hydroxylation of fatty acids and the inhibition of pro-inflammatory transcription factors (NF-κB and AP-1), pro-inflammatory cytokines (IL-1, -6, -8, -12, and TNF-α), cell4 adhesion molecules (ICAM-1 and VCAM-1), inducible nitric oxide synthase, proinflammatory nitric oxide (NO), and anti-apoptotic factors.
Epidemiological studies have suggested a correlation between chronic consumption of drinking water contaminated with arsenic and the incidence of Type 2-diabetes. The human liver after exposure to therapeutic drugs may exhibit hepatic non-cirrhotic portal hypertension, fibrosis, and cirrhosis. However, the literature provides insufficient scientific evidence to show cause and effect between arsenic and the onset of diabetes mellitus Type 2.
Diagnosis
Arsenic may be measured in blood or urine to monitor excessive environmental or occupational exposure, confirm a diagnosis of poisoning in hospitalized victims or to assist in the forensic investigation in a case of fatal over dosage. Some analytical techniques are capable of distinguishing organic from inorganic forms of the element. Organic arsenic compounds tend to be eliminated in the urine in unchanged form, while inorganic forms are largely converted to organic arsenic compounds in the body prior to urinary excretion. The current biological exposure index for U.S. workers of 35 µg/L total urinary arsenic may easily be exceeded by a healthy person eating a seafood meal.
Tests are available to diagnose poisoning by measuring arsenic in blood, urine, hair, and fingernails. The urine test is the most reliable test for arsenic exposure within the last few days. Urine testing needs to be done within 24–48 hours for an accurate analysis of an acute exposure. Tests on hair and fingernails can measure exposure to high levels of arsenic over the past 6–12 months. These tests can determine if one has been exposed to above-average levels of arsenic. They cannot predict, however, whether the arsenic levels in the body will affect health. Chronic arsenic exposure can remain in the body systems for a longer period of time than a shorter term or more isolated exposure and can be detected in a longer time frame after the introduction of the arsenic, important in trying to determine the source of the exposure.
Hair is a potential bioindicator for arsenic exposure due to its ability to store trace elements from blood. Incorporated elements maintain their position during growth of hair. Thus for a temporal estimation of exposure, an assay of hair composition needs to be carried out with a single hair which is not possible with older techniques requiring homogenization and dissolution of several strands of hair. This type of biomonitoring has been achieved with newer microanalytical techniques like Synchrotron radiation based X ray fluorescence (SXRF) spectroscopy and Microparticle induced X ray emission (PIXE).The highly focused and intense beams study small spots on biological samples allowing analysis to micro level along with the chemical speciation. In a study, this method has been used to follow arsenic level before, during and after treatment with Arsenious oxide in patients with Acute Promyelocytic Leukemia.
Chelation
Dimercaprol and dimercaptosuccinic acid are chelating agents that sequester the arsenic away from blood proteins and are used in treating acute arsenic poisoning. The most important side effect is hypertension. Dimercaprol is considerably more toxic than succimer. DMSA monoesters, e.g. MiADMSA, are promising antidotes for arsenic poisoning. Calcium sodium edetate is also used.
Nutrition
Supplemental potassium decreases the risk of experiencing a life-threatening heart rhythm problem from arsenic trioxide.
History
In addition to its presence as a poison, for centuries arsenic was used medicinally. It has been used for over 2,400 years as a part of traditional Chinese medicine. In the western world, arsenic compounds, such as salvarsan, were used extensively to treat syphilis before penicillin was introduced. It was eventually replaced as a therapeutic agent by sulfa drugs and then by other antibiotics. Arsenic was also an ingredient in many tonics (or "patent medicines").
In addition, during the Elizabethan era, some women used a mixture of vinegar, chalk, and arsenic applied topically to whiten their skin. This use of arsenic was intended to prevent aging and creasing of the skin, but some arsenic was inevitably absorbed into the blood stream.
Some pigments, most notably the popular Emerald Green (known also under several other names), were based on arsenic compounds. Overexposure to these pigments was a frequent cause of accidental poisoning of artists and craftsmen.
Arsenic became a favored method for murder of the Middle Ages and Renaissance, particularly among ruling classes in Italy allegedly. Because the symptoms are similar to those of cholera, which was common at the time, arsenic poisoning often went undetected. By the 19th century, it had acquired the nickname "inheritance powder," perhaps because impatient heirs were known or suspected to use it to ensure or accelerate their inheritances.
In ancient Korea, and particularly in Joseon Dynasty, arsenic-sulfur compounds have been used as a major ingredient of sayak (사약; 賜藥), which was a poison cocktail used in capital punishment of high-profile political figures and members of the royal family. Due to social and political prominence of the condemned, many of these events were well-documented, often in the Annals of Joseon Dynasty; they are sometimes portrayed in historical television miniseries because of their dramatic nature.
Notable cases
Arsenic poisoning, accidental or deliberate, has been implicated in the illness and death of a number of prominent people throughout history.
Francesco I de' Medici, Grand Duke of Tuscany
Recent forensic evidence uncovered by Italian scientists suggests that Francesco (1541-1587) and his wife were poisoned, possibly by his brother and successor Ferdinando.
Eric XIV of Sweden
Towards the end of his life, king Eric XIV (1533-1577) was held prisoner in many different castles in both Sweden and Finland. He died in prison in Örbyhus Castle: according to a tradition starting with Johannes Messenius, his final meal was a poisoned bowl of pea soup. A document signed by his brother, John III of Sweden, and a nobleman, Bengt Bengtsson Gylta (1514–74), gave Eric's guards in his last prison authorization to poison him if anyone tried to release him. His body was exhumed in 1958 and modern forensic analysis revealed evidence of lethal arsenic poisoning.
George III of Great Britain
George III's (1738–1820) personal health was a concern throughout his long reign. He suffered from periodic episodes of physical and mental illness, five of them disabling enough to require the King to withdraw from his duties. In 1969, researchers asserted that the episodes of madness and other physical symptoms were characteristic of the disease porphyria, which was also identified in members of his immediate and extended family. In addition, a 2004 study of samples of the King's hair revealed extremely high levels of arsenic, which is a possible trigger of disease symptoms. A 2005 article in the medical journal The Lancet suggested the source of the arsenic could be the antimony used as a consistent element of the King's medical treatment. The two minerals are often found in the same ground, and mineral extraction at the time was not precise enough to eliminate arsenic from compounds containing antimony.
Theodor Ursinus
Theodor Gottlieb Ursinus (1749–1800), a high-ranking Prussian civil servant and justice official, was poisoned by his wife Charlotte Ursinus (1760–1836). At the time, his death was ruled a stroke, but soon after the widow was found to have poisoned, between 1797 and 1801, not only her husband, but also her aunt and her lover, as well as to have attempted to poison her servant in 1803. Her sensational trial led to the first reliable method of identifying arsenic poisoning.
Napoleon Bonaparte
It has been suggested that Napoleon Bonaparte (1769–1821) suffered and died from arsenic poisoning during his imprisonment on the island of Saint Helena. Forensic samples of his hair did show high levels, 13 times the normal amount, of the element. This, however, does not prove deliberate poisoning by Napoleon's enemies: copper arsenite has been used as a pigment in some wallpapers, and microbiological liberation of the arsenic into the immediate environment would be possible. The case is equivocal in the absence of clearly authenticated samples of the wallpaper. Samples of hair taken during Napoleon's lifetime also show levels of arsenic, so that arsenic from the soil could not have polluted the post-mortem sample. Even without contaminated wallpaper or soil, commercial use of arsenic at the time provided many other routes by which Napoleon could have consumed enough arsenic to leave this forensic trace.
Simón Bolívar
South American independence leader Simón Bolívar (1783–1830), according to Paul Auwaerter from the Division of Infectious Diseases in the Department of Medicine at the Johns Hopkins University School of Medicine, may have died due to chronic arsenic poisoning further complicated by bronchiectasis and lung cancer. Auwaerter has considered murder and acute arsenic poisoning unlikely, arguing that gradual "environmental contact with arsenic would have been entirely possible" as a result of drinking contaminated water in Peru or through the medicinal use of arsenic (which was common at the time) as Bolívar had reportedly resorted to it during the treatment for some of his illnesses.
Charles Francis Hall
American explorer Charles Francis Hall (1821–1871) died unexpectedly during his third Arctic expedition aboard the ship Polaris. After returning to the ship from a sledging expedition Hall drank a cup of coffee and fell violently ill. He collapsed in what was described as a fit. He suffered from vomiting and delirium for the next week, then seemed to improve for a few days. He accused several of the ship's company, including ship's physician Emil Bessels with whom he had longstanding disagreements, of having poisoned him. Shortly thereafter, Hall again began suffering the same symptoms, died, and was taken ashore for burial. Following the expedition's return a US Navy investigation ruled that Hall had died from apoplexy.
In 1968, however, Hall's biographer Chauncey C. Loomis, a professor at Dartmouth College, traveled to Greenland to exhume Hall's body. Due to the permafrost, Hall's body, flag shroud, clothing and coffin were remarkably well preserved. Tissue samples of bone, fingernails and hair showed that Hall died of poisoning from large doses of arsenic in the last two weeks of his life, consistent with the symptoms party members reported. It is possible that he was murdered by Bessels or one of the other members of the expedition.
Clare Boothe Luce
Clare Boothe Luce (1903–1987), the American ambassador to Italy from 1953 to 1956, did not die from arsenic poisoning, but suffered an increasing variety of physical and psychological symptoms until arsenic was implicated. Its source was traced to the flaking arsenic-laden paint on the ceiling of her bedroom. She may also have eaten food contaminated by arsenic in flaking ceiling paint in the embassy dining room.
Guangxu Emperor
In 2008, testing in the People's Republic of China confirmed that the Guangxu Emperor (1871–1908) was poisoned with a massive dose of arsenic; suspects include his dying aunt, Empress Dowager Cixi, and her strongman, Yuan Shikai.
Phar Lap
The famous and largely successful New Zealand-bred racehorse Phar Lap died suddenly in 1932. Poisoning was considered as a cause of death and several forensic examinations were completed at the time of death. In a recent examination, 75 years after his death, forensic scientists determined that the horse had ingested a massive dose of arsenic shortly before his death.
King Faisal I of Iraq
According to his British nurse, Lady Badget, King Faisal I of Iraq suffered from symptoms similar to those of arsenic poisoning during his last visit to Switzerland for treatment in 1933, at the age of 48. His Swiss doctors found him in a very healthy situation a day before.
Anderson Mazoka
The popular opposition leader in Zambia, Anderson Mazoka, whose health deteriorated after the 2001 presidential elections, repeatedly accused government agents of poisoning him. His daughter, Mutinta, confirmed after his death on 24 May 2006 that arsenic was found in his body after he died from kidney complications.
