Disease Swine flu Arrival date 27 April 2009 Deaths 214 (19 November 2009) | Virus strain H1N1 Origin Central Mexico | |
 | ||
The 2009 flu pandemic was a global outbreak of a new strain of influenza A virus subtype H1N1, first identified in April 2009, termed Pandemic H1N1/09 virus by the World Health Organization (WHO) and colloquially called swine flu. The outbreak was first observed in Mexico, and quickly spread globally. On 11 June 2009, the WHO declared the outbreak to be a pandemic. The overwhelming majority of patients experience mild symptoms", but some persons are in higher risk groups, such as those with asthma, diabetes, obesity, heart disease, or who are pregnant or have a weakened immune system. In the rare severe cases, around 3–5 days after symptoms manifest, the sufferer's condition declines quickly, often to the point of respiratory failure.
Contents
- Reported cases
- Detailed reports
- Public information
- Control measures
- Travel to and from affected areas
- Preparations
- Genetic analysis
- Diagnosis
- Hygiene recommendations
- Immunity
- Vaccine
- Possible use of face masks
- References
The virus reached the United Kingdom in April 2009. The first cases were confirmed on 27 April 2009 in passengers returning from Mexico. The first case of person to person transmission within the UK was announced on 1 May 2009. In the UK, 5- to 14-year-olds are the age group predominantly affected. Laboratory tests have demonstrated that older people have some immunity.
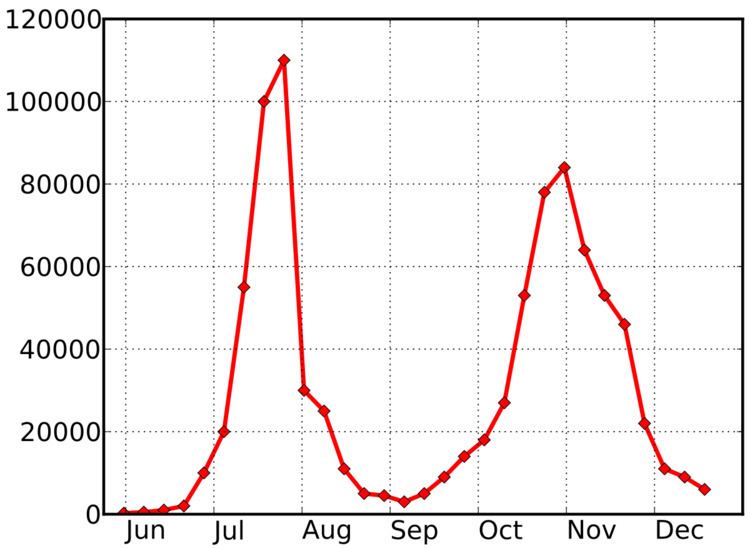
After a slow start, the virus spread rapidly in the UK in July 2009, with new cases peaking at 110,000 in the last week of that month, according to The Health Protection Agency's modelling estimate, but declining sharply in the first week of August 2009. Cases fell progressively down to 3,000 in the first week of September 2009, then began to rise again. The decline in cases during the summer had been predicted, but a large surge was expected in the autumn to coincide with the normal flu season. Cases rose to 84,000 by the end of October, well below the summer's peak and then declined during November.
Reported cases
Until 2 July 2009 the HPA published daily reports of laboratory-confirmed cases with breakdown by region, by age, and by source of infection (travel, community, etc.). From that date routine laboratory testing of all suspected cases and reporting of figures was discontinued. As of 8 July 2009 figures shown in this article are laboratory confirmed cases reported on 2 July.
Deaths are often reported as occurring "after contracting the swine flu virus" without flu being necessarily the cause of death of people with underlying health problems.
Researchers at Imperial College London said in July 2009 that the best estimate was that about 0.5% of those who get swine flu bad enough to seek medical help die from it, a figure very similar to the estimate for seasonal influenza.
Detailed reports
On 25 April 2009, a member of British Airways cabin crew was taken to Northwick Park Hospital in Harrow and quarantined after falling ill with flu-like symptoms on a flight from Mexico City though he was later found not to have swine flu.
On 26 April, two people were admitted to Monklands Hospital in Airdrie, North Lanarkshire, with mild flu-like symptoms after returning from Mexico. The next day, the Cabinet Secretary for Health and Wellbeing, Nicola Sturgeon, confirmed that these were cases of the swine influenza A (H1N1) virus. Authorities in both Scotland and England stated that there were no plans to trace the fellow airline passengers who may have travelled alongside the couple, since the authorities do not classify them as "close contacts". These cases along with one in Spain are the first confirmed cases in Europe.
At noon on 29 April the government reported three more confirmed cases in the UK, including the first cases in England. All three had recently returned from Mexico. The secondary school, Paignton Community and Sports College, closed for seven days.
By 26 May the number of people who had contracted the disease in-country increased to 125, the highest in Europe and triple the second highest, Spain.
On 28 May, sixty four people connected with a primary school in Birmingham were diagnosed with swine flu .
On 8 June the HPA issued a report stating that the majority of cases are in school age children and young adults, which has not been the case in most pandemics with the notable exception of 1918.
On 25 June the chief medical officer Sir Liam Donaldson said certain areas were seeing rapid community spread which meant that it was no longer practical to attempt in those areas (initially parts of London, the west Midlands and east Berkshire) to put a ring around the outbreaks by tracing the people with whom confirmed cases have come into contact and giving them drugs to try to prevent flu developing. In these areas, anti-viral drugs may in the future only be given to people showing symptoms, and tracing of contacts will stop. The contingency plans always envisaged the containment phase would not last indefinitely. The start of the treatment (as against containment) approach was announced on 2 July 2009.
Every year in late June and early July the Wimbledon tennis championships are held in London, attracting worldwide interest and with many hours of UK television coverage every day. On 1 July 2009 it was reported that 28 Wimbledon staff had been asked to stay at home with flu-like symptoms. Two named players are reported to have caught the virus.
A study published in the August 2009 issue of The Lancet (available on 20 July) suggests that prolonging the school holidays could reduce the spread of the virus by up to 17%. This would be disruptive, and would not reduce the overall number of infections, but could delay the spread and buy time for preparation of a vaccine. The government's advice is that schools should not be closed, but that the evidence will be reviewed in August as school summer holidays end.
Public information
The Department of Health announced on 29 April 2009 that they intended to send an information leaflet on swine flu to every household in the UK. The information leaflets were distributed at the beginning of May. On 29 April, Alan Johnson announced that television and radio advice would also be broadcast starting on 30 April. On 30 April 2009, a swine flu information line was launched with advice on setting up "flu friends" (this is not the National Flu Line service mentioned below).
The Department of Health Pandemic Plan (revised November 2007) states "UK health departments (directorate in Scotland) will run a national door drop and advertising campaign in Phase 5, alerting the public to the heightened risk, emphasising the need for personal preparation and socially responsible behaviour. A public information film will demonstrate how to slow the spread of the virus, and the National Flu Line service will be available. Information materials will also be available through primary care, pharmacies and on the Department of Health website." After criticism of the lateness of its launch, it was announced in late July that the National Flu Line service was to be launched on 24 July 2009.
There are government websites with general information and the latest updates on human swine flu in England, Northern Ireland, Scotland, and Wales.
The HPA website includes frequently updated advice for the public, advice on exclusion from schools and workplaces (and a document specifically for schools), and information for health professionals.
During the initial containment phase of the swine flue outbreak the HPA published detailed information in daily and weekly reports linked from its Epidemiological data page on its website. On 2 July, when the policy of containment was dropped in favour of treatment of presumed cases, the daily updates of laboratory confirmed cases were stopped. A weekly epidemiological update and pandemic flu update are published each Tuesday, with much detailed information including regional information and breakdown by age.
Control measures
On 11 May 2009 UK epidemiologists at Imperial College London considered that H1N1 swine flu was spreading fast enough to justify the preparations for a pandemic. It was showing "sustained human-to-human transmission", thereby justifying the WHO's pandemic phase 5 rating. It is estimated that on average each person who contracts flu passes it on to between 1.4 and 1.6 other people, no worse than the three influenza pandemics of the twentieth century. Early analysis suggested that the spread was likely to be similar to the earlier pandemics. Up to the date of the study, clinical severity was similar to 1957 and less than 1918 flu pandemic. However, the clinical severity of the outbreak and how the virus will evolve cannot yet be predicted.
Travel to and from affected areas
On 27 April, the Foreign & Commonwealth Office advised against all but essential travel to Mexico and stated that British citizens in Mexico... "may wish to consider whether they should remain in Mexico at this time". On 28 April the Mexican Tourist Board estimated that there were "a few thousand" British tourists in Mexico.
Holiday companies Thomas Cook and Airtours said that between them they had about "3,000 holidaymakers in Mexico" as of 28 April 2009. The first British tourists being brought back early from Mexico on 28 April 2009 told reporters that they had received little or no information about health precautions, either from the Mexican authorities, hotels, or from local tour guides.
A leaflet is being distributed at all ports of entry into the UK providing passengers arriving in the UK with information on swine flu.
Until 21 May HPA staff met travellers arriving from Mexico. This was discontinued on 22 May, but advice remained that travellers from affected areas who become unwell within seven days of arrival, and contacts with symptoms of a confirmed or probable case, should stay at home and contact their GP or NHS Direct. Contact tracing of passengers deemed to be at risk of swine flu will be carried out on the basis of risk, as for other communicable diseases.
Preparations
Information, advice, and guidance both general and for specific cases (schools, workplaces) is being made available and updated by the HPA (see Public information campaign section above).
As of 13 June 2009 the government estimated that the UK has enough anti-viral drugs for 50% of the population but has plans to raise that figure to 80%.
There is a pandemic plan covering topics from distributing the drugs and setting up helplines to closing schools and banning public events which was tested in a large exercise in 2007. There is also a specific response plan for London. Oseltamivir (Tamiflu) and zanamivir (Relenza), the two anti-virals known to be effective, must be taken within 48 hours of onset of symptoms or earlier to be effective; the positive effects are greatest if treatment is started within six hours.
The HPA reported in its 24 June 2009 weekly epidemiological report that all 17 samples of the virus laboratory tested for resistance that week were found to be sensitive to oseltamivir and zanamivir, but resistant to amantadine. The first case of resistance of the virus to oseltamivir, in Denmark, was reported on 29 June 2009.
On 5 May 2009 plans were announced for pupils unable to sit examinations at schools affected by flu to be assessed in other ways to ensure that children are not disadvantaged.
The Department of Health has listed all the pandemic flu guidance that it had published as of 8 June 2008.
Genetic analysis
Samples from suspected cases have been analysed by the National Institute for Medical Research in London, which is also examining samples of the U.S. strain of the disease.
By 8 May 2009 the US Centers for Disease Control and Prevention had made genetic information on the swine flu virus available, and the virus from European samples had been isolated and its full genetic fingerprint determined by UK researchers. The genetics and effects of the virus in general are discussed in the article on the 2009 swine flu outbreak.
Diagnosis
The fastest way for laboratory confirmation of swine flu is by the PCR method, described as a real-time method. According to the World Health Organization there are four laboratories in the UK able to perform PCR to diagnose influenza A (H1N1) virus infection in humans: Regional Virus Laboratory, Royal Victoria Hospital, Belfast, NI; Regional Virus Laboratory, Gartnavel General Hospital, Glasgow, Scotland; Health Protection Agency, Centre for Infections, Enteric, Respiratory, & Neurological Virus Laboratory, London; WHO Collaborating Centre for Reference and Research on Influenza, National Institute for Medical Research, London.
Another laboratory confirmation is a fourfold increase in virus-specific antibodies 10 to 14 days later.
From 2 July 2009 when a treatment, rather than containment, approach was adopted, the official clinical diagnostic criteria became: "fever (pyrexia ≥38 °C) or a history of fever, and also influenza-like illness (two or more of the following symptoms: cough; sore throat; rhinorrhoea; limb or joint pain; headache; vomiting or diarrhoea) or severe and/or life-threatening illness suggestive of an infectious process".
Professor Neil Ferguson, an epidemiologist at Imperial College London, who advises the Government and the World Health Organisation, said on 8 June 2009 that HPA statistics were at best accounting for half of cases.
In the USA mathematical modelling based on surveys estimated that there were about 1 million cases of H1N1 flu on 25 June 2009, compared to 28,000 reported officially. Such a study has not been carried out in the UK.
As of 2 July 2009 GPs will diagnose based on clinical observation and routine swabbing will stop, and the HPA will "no longer be providing a daily update of the numbers of cases confirmed through laboratory tests"
Hygiene recommendations
According to the Health Protection Agency's "Swine flu: frequently asked questions" web page, transmission of this new virus is thought to occur in the same way as seasonal flu:
When the issue of touching your eyes, nose or mouth is combined with other infection control practices and good hygiene measures as recommended by the Health Protection Agency's website, the following recommendations emerge as important ways to help reduce the spread of swine flu and other viruses:
For people belonging to a high-risk group it is particularly important that they start taking anti-virals as soon as possible after infection. High-risk groups include people with long-term conditions, those over 65, children under five and pregnant women.
Immunity
A study at the U.S. Centers for Disease Control and Prevention published in May 2009 found that children had no pre-existing immunity to the new strain but that adults, particularly those over 60, had some degree of immunity. Children showed no cross-reactive antibody reaction to the new strain, adults aged 18 to 64 had 6–9%, and older adults 33%. The large proportion of cases in the UK affecting children and young adults is consistent with this pattern of resistance.
Vaccine
The usual seasonal flu vaccines give little or no immunity against the new strain of flu. There is an international program to produce a vaccine which will be effective against the new H1N1 strain. The chief medical officer Sir Liam Donaldson said on 25 June that it seemed likely that the UK would receive the first batches of vaccines slightly earlier than expected, possibly from August rather than the autumn as first expected, although some industry sources do not expect supplies to be available so soon. The government has contracts for 132 million doses. There are risks involved in shifting resources to the new vaccine: it will not be possible to produce the seasonal flu vaccine, and it is possible that the virus will mutate to make a vaccine developed before the mutation ineffective.
Possible use of face-masks
The then Health Secretary Alan Johnson told MPs on 27 April that "Although we are aware that face-masks are being given out to the public in Mexico, the available scientific evidence does not support the general wearing of face-masks by those who are not ill, whilst going about their normal activities."
Professor Steve Field, chairman of the Royal College of General Practitioners, said people in the UK were "perfectly safe at the moment", and did not need to start wearing face-masks or stop eating pork.
The Head of Pandemic Planning at the Royal College of General Practitioners, Dr Maureen Baker, stated on 27 April that "Masks become ineffective when they become damp or after a few hours. There has been a lot of debate on the use of face-masks and some authorities say that, in the community, the most effective use is to give to patients who may have symptoms when they present in the surgery – that should help reduce the infectivity of that patient to surgery staff and other patients. I expect the Department of Health will issue guidance on use of face-masks if we move into a pandemic phase." Masks may not protect the wearer from inhalation of the virus, but might protect other people from picking up the virus from the wearer.
Professor John Oxford, a virologist at leading London hospital, The Barts and the London, said: "Really, there is very little evidence that masks actually offer much protection against flu."
It was reported that the UK government was urgently seeking to acquire more face-masks.
The advice given by authorities in several countries on the use of face masks has been summarised in an article, with many references, published on 4 June 2009.
Aside from their obligations under health and safety legislation, employers can help to minimise the spread of the virus and support good infection control practice by positively encouraging any employee who reports feeling unwell with influenza-like symptoms to stay at home until their symptoms resolve, by sending people home who develop influenza-like illness at work (avoiding public transport and wearing a face mask if possible) and by ensuring that stocks of surgical face-masks are available in the workplace for symptomatic staff to wear until they get home.
