Entrez 4018 | Ensembl ENSG00000198670 | |
 | ||
External IDs HomoloGene: 87856 GeneCards: LPA | ||
Lipoprotein(a) (also called Lp(a) or LPA) is a lipoprotein subclass. Genetic studies and numerous epidemiologic studies have identified Lp(a) as a risk factor for atherosclerotic diseases such as coronary heart disease and stroke.
Contents
- Structure
- Catabolism and clearance
- Populations
- Function
- Pathology
- Lipoproteina and disease
- Diagnostic testing
- Treatment
- Interactions
- References
Lipoprotein(a) was discovered in 1963 by Kåre Berg and the human gene encoding apolipoprotein(a) was cloned in 1987.
Structure
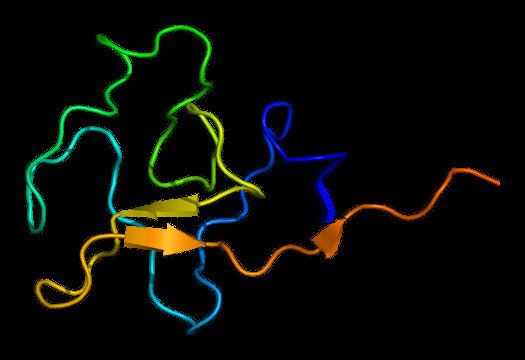
Lipoprotein(a) [Lp(a)] consists of an LDL-like particle and the specific apolipoprotein(a) [apo(a)], which is covalently bound to the apoB of the LDL like particle. Lp(a) plasma concentrations are highly heritable and mainly controlled by the apolipoprotein(a) gene [LPA] located on chromosome 6q26-27. Apo(a) proteins vary in size due to a size polymorphism [KIV-2 VNTR], which is caused by a variable number of so-called kringle IV repeats in the LPA gene. This size variation at the gene level is expressed on the protein level as well, resulting in apo(a) proteins with 10 to > 50 kringle IV repeats (each of the variable kringle IV consists of 114 amino acids). These variable apo(a) sizes are known as "apo(a) isoforms". There is a general inverse correlation between the size of the apo(a) isoform and the Lp(a) plasma concentration One theory for the size/plasma level correlation involves difference rates of protein synthesis. There appears to be a relationship between the number of kringle repeats and the processing time of the precursor apo (a) protein. That is, the larger the isoform, the more apo(a) precursor protein accumulates intracellularly in the endoplasmic reticulum. Lipoprotein (a) is not fully synthesized until the precursor protein is released from the cell, so the slower rate of production for the larger isoforms limits the plasma concentration.
Apo(a) is expressed by liver cells (hepatocytes), and the assembly of apo(a) and LDL particles seems to take place at the outer hepatocyte surface. The half-life of Lp(a) in the circulation is about 3 to 4 days.
Catabolism and clearance
The mechanism and sites of Lp(a) catabolism are largely unknown. Uptake via the LDL receptor is not a major pathway of Lp(a) metabolism. The kidney has been identified as playing a role in Lp(a) clearance from plasma.
Populations
Lp(a) concentrations vary over one thousandfold between individuals, from <0.2 to > 200 mg/dL. This range of concentrations is observed in all populations studied so far. The mean and median concentrations between different world populations show distinct particularities, the main being the two- to threefold higher Lp(a) plasma concentration of populations of African descent compared to Asian, Oceanic, or European populations. The general inverse correlation between apo(a) isoform size and Lp(a) plasma concentration is observed in all populations. However, mean Lp(a) associated with certain apo(a) isoforms varies between populations.
Function
Lp(a) is assembled at the hepatocyte cell membrane surface, while other scenarios exist with regard to the location of assembly. It mainly exists in plasma. Lp(a) contributes to the process of atherogenesis. Because of its structural similarity to plasminogen and tissue plasminogen activator, competitive inhibition leads to reduced fibrinolysis, and as a result of the stimulation of secretion of plasminogen activator inhibitor 1, Lp(a) leads to thrombogenesis. It may also enhance coagulation by inhibiting the function of tissue factor pathway inhibitor. Lp(a) carries cholesterol and binds atherogenic proinflammatory oxidized phospholipids as a preferential carrier of oxidized phospholipids in human plasma, which attract inflammatory cells to vessel walls and leads to smooth muscle cell proliferation. Moreover, Lp(a) is also hypothesized to be involved in wound healing and tissue repair, interacting with components of the vascular wall and extra cellular matrix. Apo(a), a distinct feature of the Lp(a) particle, binds to immobilized fibronectin and endows Lp(a) with the serine-proteinase-type proteolytic activity.
However, individuals without Lp(a) or with very low Lp(a) levels seem to be healthy. Thus, plasma Lp(a) is not vital, at least under normal environmental conditions. Since apo(a)/Lp(a) derived rather recently in mammalian evolution - only old world monkeys and humans have been shown to harbour Lp(a) - its function might not be vital but just evolutionarily advantageous under certain environmental conditions, e.g. in case of exposure to certain infectious diseases.
Another possibility, suggested by Linus Pauling, is that Lp(a) is a primate adaptation to L-gulonolactone oxidase (GULO) deficiency, found only in certain lines of mammals. GULO is required for converting glucose to ascorbic acid (vitamin C), which is needed to repair arteries; following the loss of GULO, those primates that adopted diets less abundant in vitamin C may have used Lp(a) as an ascorbic-acid surrogate to repair arterial walls.
Pathology
The structure of lipoprotein (a) is similar to plasminogen and tPA (tissue plasminogen activator) and it competes with plasminogen for its binding site, leading to reduced fibrinolysis. Also, because Lp(a) stimulates secretion of PAI-1, it leads to thrombogenesis. Lp(a) also carries cholesterol and thus contributes to atherosclerosis. In addition, Lp(a) transports the more atherogenic proinflammatory oxidized phospholipids, which attract inflammatory cells to vessel walls, and leads to smooth muscle cell proliferation.
Lipoprotein(a) and disease
High Lp(a) in blood is a risk factor for coronary heart disease (CHD), cardiovascular disease (CVD), atherosclerosis, thrombosis, and stroke. The association between Lp(a) levels and stroke is not as strong as that between Lp(a) and cardiovascular disease. Lp-a concentrations may be affected by disease states (for example kidney failure), but are only slightly affected by diet, exercise, and other environmental factors. Most commonly prescribed lipid-reducing drugs have little or no effect on Lp(a) concentration. Results using statin medications have been mixed in most trials, although a meta-analysis published in 2012 suggests that atorvastatin may be of benefit. Niacin VitaminB3 (nicotinic acid) and aspirin are two relatively safe, easily available and inexpensive drugs known to significantly reduce the levels of Lp(a) in some individuals with high Lp(a); they should be used under the supervision of a qualified physician.
High Lp(a) predicts risk of early atherosclerosis independently of other cardiac risk factors, including LDL. In patients with advanced cardiovascular disease, Lp(a)indicates a coagulant risk of plaque thrombosis. Apo(a) contains domains that are very similar to plasminogen (PLG). Lp(a) accumulates in the vessel wall and inhibits binding of PLG to the cell surface, reducing plasmin generation, which increases clotting. This inhibition of PLG by Lp(a) also promotes proliferation of smooth muscle cells. These unique features of Lp(a) suggest Lp(a) causes generation of clots and atherosclerosis.
Vegetarians have higher levels of Lp-a than fish eaters in one homogeneous tribal population of Tanzania raising the possibility that pharmacologic amounts of fish oil supplements may be helpful to lower the levels of Lp-a.
Some studies have shown that regular consumption of moderate amounts of alcohol leads to significant decline in plasma levels of Lp-a while other studies have not.
Diagnostic testing
Numerous studies confirming a strong correlation between elevated Lp(a) and heart disease have led to the consensus that Lp(a) is an important, independent predictor of cardiovascular disease. Animal studies have shown that Lp(a) may directly contribute to atherosclerotic damage by increasing plaque size, inflammation, instability, and smooth muscle cell growth. Genetic data also support the theory that Lp(a) causes cardiovascular disease.
The European Atherosclerosis Society currently recommends that patients with a moderate or high risk of cardiovascular disease have their lipoprotein (a) levels checked. Any patient with one of the following risk factors should be screened;
If the level is elevated, treatment should be initiated with a goal of bringing the level below 50 mg/dL. In addition, the patient's other cardiovascular risk factors (including LDL levels) should be optimally managed. Apart from the total Lp(a) plasma concentration, the apo(a) isoform might be an important risk parameter as well.
Prior studies of the relationship between LP(a) and ethnicity have shown inconsistent results. Lipoprotein (a) levels seem to differ in different populations. For example, in some African populatation, Lp(a) levels are, on average higher, than other groups, so that using a risk threshold of 30 mg/dl would classify up to > 50% of the individuals as higher risk. Some part of this complexity may be related to the different genetic factors involved in determining Lp(a) levels. One recent study showed that in different ethnic groups, different genetic alterations were associated with increased Lp(a) levels.
More recent data suggest that prior studies were under-powered. The Atherosclerosis Risk in Communities (ARIC) followed 3467 African Americans and 9851 whites for 20 years. The researchers found that an elevated Lp(a) conferred the same risk in each group. However, African Americans had roughly three times the level of Lp(a), and Lp(a) also predicted an increased risk of stroke.
Approximate levels of risk are indicated by the results below, although at present there are a variety of different methods by which to measure Lp(a). A standardized international reference material has been developed and is accepted by the WHO Expert Committee on Biological Standardization and the International Federation of Clinical Chemistry and Laboratory Medicine. Although further standardization is still needed, development of a reference material is an importance step towards standardizing results.
Lipoprotein(a) - Lp(a)
Desirable: < 14 mg/dL (< 35 nmol/L)Borderline risk: 14 - 30 mg/dL (35 - 75 nmol/L)High risk: 31 - 50 mg/dL (75 - 125 nmol/L)Very high risk: > 50 mg/dL (> 125 nmol/L)LP(a) appears with different isoforms (per kringle repeats) of apolipoprotein - 40% of the variation in Lp(a) levels when measured in mg/dl can be attributed to different isoforms. Lighter Lp(a) are also associated with disease. Thus a test with simple quantitative results may not provide a complete assessment of risk.
Treatment
At the current time, the simplest treatment for an elevated lipoprotein(a) is niacin, 1-3 grams daily, in general in an extended-release form. Niacin therapy can reduce lipoprotein(a) levels by 20-30%. A more effectve treatment is the Linus Pauling protocol: 6-18 grams/day ascorbic acid, 6 grams/day L-lysine and 2 grams/day L-proline. This protocol can reduce LP(a) 2-5 fold over a few months. Aspirin may be beneficial, as well, but has only been tested in patients that carry the apolipoprotein(a) gene minor allele variant (rs3798220). A recent meta-analysis suggests that atorvastatin may also lower Lp(a) levels. In severe cases, such as familial hypercholesterolemia, or treatment resistant hypercholesterolemia, lipid apheresis may result in dramatic reductions of lipoprotein(a). The goal of treatment is to reduce levels to below 50 mg/dL.
Other medications that are in various stages of development include thyromimetics, cholesterol-ester-transfer protein (CETP inhibitors), anti-sense oligonucleopeptides, and proprotein convertase subtilisin/kexin type 9 (PCSK-9) inhibitors. L-carnitine may also reduce lipoprotein a levels. TRT (testosterone replacement therapy) also causes Lp(a) to drop.
Gingko biloba may be beneficial, but has not been clinically verified. Coenzyme Q-10 and pine bark extract have been suggested as beneficial, but neither has been proven in clinical trials.
Testosterone is known to reduce lipoprotein(a) levels. Testosterone replacement therapy also appears to be associated with lower lipoprotein(a) levels. One large study suggested that there was a decreased association between lipoprotein(a) levels and risk. Estrogen as a prevention strategy for heart disease is current topic of much research and debate. Risks and benefits may need to be considered for each individual. At present, estrogen is not indicated for treatment of elevated lipoprotein(a). Tamoxifen and raloxifene have not been shown to reduce levels.
The American Academy of Pediatrics now recommends that all children be screened for cholesterol between the ages of 9 and 11. Lipoprotein(a) levels should be considered in particular in children with a family history of early heart disease or high blood cholesterol levels. Unfortunately, there have not been enough studies to determine which therapies might be beneficial.
Interactions
Lipoprotein(a) has been shown to interact with Calnexin, Fibronectin and Fibrinogen beta chain.
