Specialty medical genetics DiseasesDB 4143 eMedicine article/154555 | ICD-10 Q21.8 MedlinePlus 007317 | |
 | ||
ICD-9-CM 745.4 (CDC/BPA 745.410) | ||
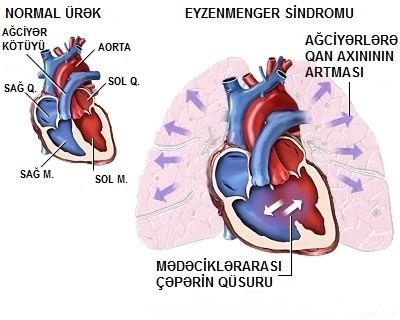
Eisenmenger's syndrome (or ES, Eisenmenger's reaction, Eisenmenger physiology, or tardive cyanosis) is defined as the process in which a long-standing left-to-right cardiac shunt caused by a congenital heart defect (typically by a ventricular septal defect, atrial septal defect, or less commonly, patent ductus arteriosus) causes pulmonary hypertension and eventual reversal of the shunt into a cyanotic right-to-left shunt. Because of the advent of fetal screening with echocardiography early in life, the incidence of heart defects progressing to Eisenmenger's has decreased.
Contents
Eisenmenger's syndrome in a pregnant mother can cause serious complications, though successful delivery has been reported. Maternal mortality ranges from 30% to 60%, and may be attributed to fainting spells, thromboembolism, hypovolemia, hemoptysis or preeclampsia. Most deaths occur either during or within the first weeks after delivery. Pregnant women with Eisenmenger syndrome should be hospitalized after the 20th week of pregnancy - or earlier if clinical deterioration occurs.
Etymology
Eisenmenger syndrome was so named by Dr. Paul Wood after Dr. Victor Eisenmenger, who first described the condition in 1897.
Signs and symptoms
Signs and symptoms of Eisenmenger syndrome include the following:
Causes
A number of congenital heart defects can cause Eisenmenger syndrome, including atrial septal defects, ventricular septal defects, patent ductus arteriosus, and more complex types of acyanotic heart disease.
Pathogenesis
The reason Eisenmenger's syndrome often presents later in life can be explained by alterations of the normal physiology of the heart and the maladaptive responses that occur over time. The larger and more muscular left side of the heart must generate the high pressure required to supply blood to the extensive, high-resistance systemic circulation. In contrast, the smaller, right side of the heart must generate a much lower pressure in order to pass blood through the low-resistance, high compliance circulation of the lungs. The lungs are able to accomplish this low-resistance circulation largely due to the fact that the length of the pulmonary circulation is smaller, and because much of the circuitry is in parallel rather than in series.
If a significant anatomic defect (i.e. a hole or breach) exists between the two sides of the heart, a shunt will occur, causing blood to flow down the normal pressure gradient from the left side to the right side. The amount of blood shunted is proportional to the size of the defect, and the beat-to-beat volume of blood pumped through a left-to-right breach is a percentage of anticipated cardiac output (CO) of the left ventricle. Clinically a low index or percentage of CO ejected through a shunt is harmless; a high index or percentage of CO ejected through a left-to-right shunt heralds Eisenmenger's physiology.
The left-to-right shunting of blood results in abnormally high blood flow and pressure directed to the right heart circulation, gradually leading to maladaptive changes that ultimately result in pulmonary hypertension. Increased right-sided blood volume and pressure causes a cascade of pathologic damage to the delicate pulmonary capillaries, causing them to be incrementally replaced with scar tissue. Scar (dead lung tissue) does not contribute to oxygen transfer, therefore decreasing the useful volume of the pulmonary vasculature. The scar tissue also provides less flexibility and compliance than normal lung tissue, causing further increases in pulmonary blood pressure, and the weakened heart must pump harder to continue supplying the lungs, leading to damage of more capillaries. It is because of this maladaptive response that at the onset of Eisenmenger's syndrome, the damage is considered irreversible, even if the underlying heart defect is corrected after the fact.
Eventually, due to increased resistance and decreased compliance of the pulmonary vessels, elevated pulmonary pressures cause the myocardium of the right heart to hypertrophy (RVH). The onset of Eisenmenger's syndrome begins when right ventricular hypertrophy causes right heart pressures to exceed that of the left heart, leading to reversal of blood flow through the shunt (i.e., blood moves from the right side of the heart to the left side). As a consequence, deoxygenated blood returning from the body bypasses the lungs through the reversed shunt and proceeds directly to systemic circulation, leading to cyanosis and resultant organ damage.
The defect, now a right-to-left shunt, causes reduced oxygen saturation in the arterial blood due to mixing of oxygenated blood returning from the lungs with the deoxygenated blood returning from systemic circulation. This decreased saturation is sensed by the kidneys, resulting in a compensatory increase in erythropoietin production and an increased production of red blood cells in an attempt to increase oxygen delivery. As the bone marrow increases erythropoiesis, the systemic reticulocyte count and the risk for hyperviscosity syndrome increases. Reticulocytes are less efficient at carrying oxygen as mature red cells, and they are less deformable, causing impaired transit through capillary beds. This contributes to the death of pulmonary capillary beds.
A person with Eisenmenger's syndrome is paradoxically subject to the possibility of both uncontrolled bleeding due to damaged capillaries and high pressure, as well as spontaneous clots due to hyperviscosity and stasis of blood.
Treatment
If the inciting defect in the heart is identified before it causes significant pulmonary hypertension, it can normally be repaired through surgery, preventing the disease. After pulmonary hypertension is sufficient to reverse the blood flow through the defect, however, the maladaptation is considered irreversible, and a heart–lung transplant or a lung transplant with repair of the heart is the only curative option. Transplantation is the final therapeutic option and only for patients with poor prognosis and quality of life. Timing and appropriateness of transplantation remain difficult decisions. 5-year and 10-year survival ranges between 70% and 80%, 50% and 70%, 30% and 50%, respectively. Since the average life expectancy of patients after lung transplantation is as low as 30% at 5 years, patients with reasonable functional status related to Eisenmenger syndrome have improved survival with conservative medical care compared with transplantation.
Various medicines and therapies for pulmonary hypertension are under investigation for treatment of the symptoms.
